Periodontal Disease and Rheumatoid Arthritis – Controlling Two Birds with One Stone?
By: Pete Williams, M.Med.Sci, CSCS, IFMCP
September 10, 2021
The Challenge:
Our case study represents an example of the emerging evidence from interventional and, more recently, animal studies showing how seemingly unrelated diseases such as periodontal disease and rheumatoid arthritis can be related through similar genetic, biological, and clinically consistent mechanisms.1,2,3,4.
The Background:
- Age: 57 years old
- Sex: F
- Medical History: Diagnosis of Palindromic Rheumatism, elevated hs-CRP 26.2, APOE3/3, stool test indications of possible SIBO, comprehensive testing results revealing Vitamin B concerns.
- Periodontal Assessment: Generalized plaque, high level of bleeding on probing, generalized bone loss of approximately 40% with probe depths ranging from 2mm-7 mm with furcation involvement. Extremely elevated rate of collagen breakdown and high levels of a biomarker activated MMP-8 (43.16 ng/ml). (ideally < 20 ng/ml)
Medical Assessment: The right-side extremities have been impacted with the knee having a large Baker’s Cyst, swollen right ankle with a reduction in feeling in the foot, reduced range of motion overall and stiffness in right wrist and several finger joints in both hands.
The Solution:
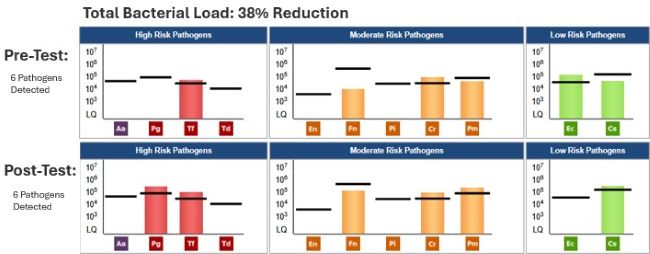
- Date of MyPerioPath® (Pre-Therapy) Test: 7/7/2020
- Periodontal Therapy: Guided biofilm therapy every 2-3 months,
- Medical Therapy: Anti-inflammatory focus with curcumin 500 mg bid, Omega 3 oil 2.5g, increase phytochemical density with a variety of real whole food, green tea and collagen.
- Home Care: Re-mineralizing toothpaste and antiseptic mouthwash, TePe™ brushes (interdental), floss twice a day and brush twice a day with an electric toothbrush. A tongue scraper in the evening was introduced.
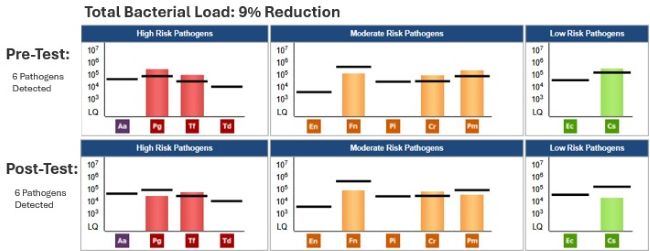
- Date of MyPerioProgress® (post-therapy test): 9/22/2020 and 11/17/2020
The Result:
At 8 weeks post dental and functional medicine treatment, the patient observed a decrease in swelling and joint soreness, especially in her hands and wrists. Her perception of daily pain significantly reduced. The Baker’s cyst reduced in size approximately 50%. CRP dramatically improved, reducing from 26.2 to 4.8. With the increased bacterial load but reduced disease activity (MMP8 40-MMP8 <10), we theorize that, based on the oral genomic data, more bacterial interventions will continue to calm local and systemic inflammation and modulate acquired immunity, continuing to reduce active periodontal disease and systemic inflammation.
About the Author:

Founder of Functional Medicine Associates, Pete is an exercise and medical scientist. In 2002, he was part of the UK’s founding group of Certified Strength and Conditioning Specialists, as accredited by the National Strength and Conditioning Association of America. In 2004, he became the youngest ever recipient of a ‘Lifetime Achievement’ award from the Register for Exercise Professionals. In 2013, he was in the first worldwide cohort to be awarded the Institute for Functional Medicine Certified Practitioner status and has represented the Institute for Functional Medicine as a Clinical Innovator.
Pete has had over 20 years of experience applying Functional Medicine in clinical practice and is seen by his peers as one of the leading figures in Functional Medicine in the UK. He is a sought-after speaker and advisor to nutraceutical and lab testing companies. Throughout this time, he has treated people with a wide range of chronic diseases.