The Consequences of Oral Bacteria and Gum Disease Go Far Beyond the Mouth
Author: Dr. Ron McGlennen
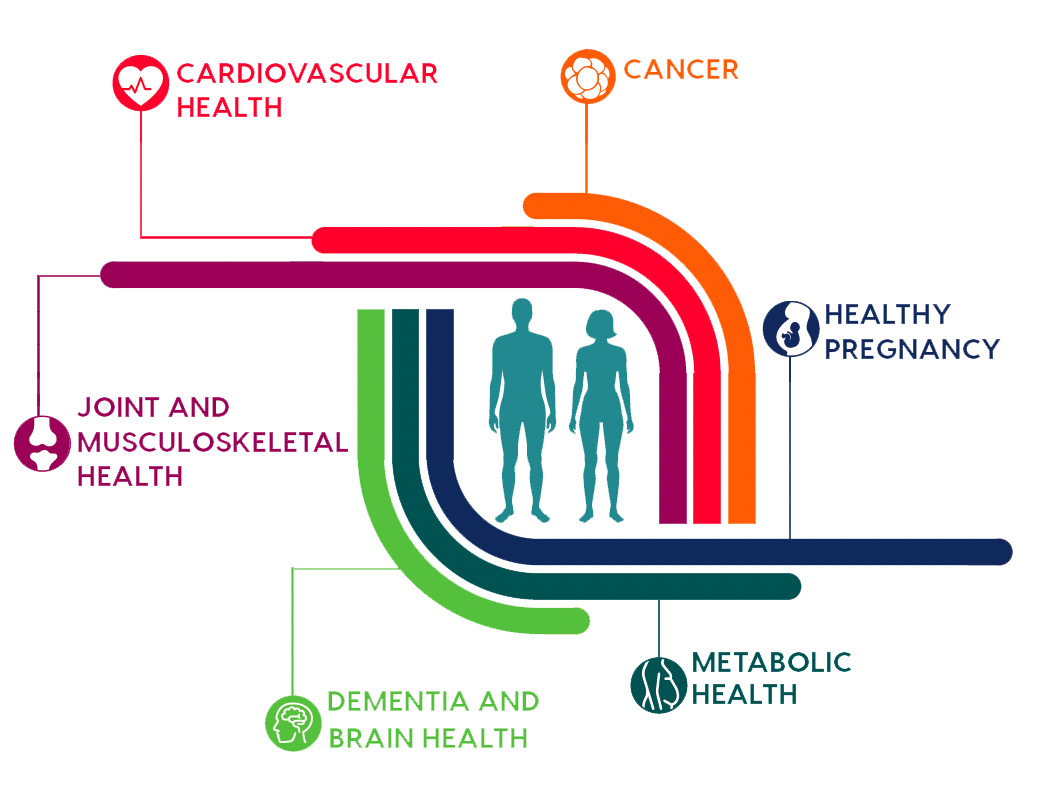
OralDNA® Labs offers testing for the profile of oral bacteria that cause periodontal disease. These bacteria, especially at high levels, and in combination with an individual’s genetic inflammatory response, result in bad breath, painful, bleeding gums, loss of bone and eventually tooth loss. But the consequences of these same bacteria, present for years and decades, add significantly to the risk of wide range of life- threatening diseases beyond the mouth. Below are some of those diseases and the measurable risk of those diseases becoming serious if these oral pathogens are not treated.
Cardiovascular disease: ![]()
![]()
![]()
![]()
![]()
![]() There is consensus within the medical and dental professional organizations that periodontal bacteria contribute to the initiation, progression and prognosis of cardiovascular disease. From key meta-analysis studies, persons with untreated periodontal infections have up to a 20% increase in their risk of coronary vascular disease1. The multiple of risk for stroke (1.74-2.85 fold) and peripheral vascular disease (1.41-2.27 fold) is equal or greater1. More specifically, the risk of a first myocardial infarction is associated with periodontal disease (OR of 1.49) even after adjustment for a history of smoking, obesity, diabetes and selected socioeconomic factors2. But equally important is the concern for specific bacteria that are a basis for this risk including A.a., P.g., T.f., T.d., F.n. and P.i.3-7. Specifically, Fn carries a series of virulence factors that can contribute to inflammation of the arterial wall8. Toward the interest to prevent heart and vascular disease, testing your patients for which types and what levels of these dangerous bacteria are present will provide them better care.
There is consensus within the medical and dental professional organizations that periodontal bacteria contribute to the initiation, progression and prognosis of cardiovascular disease. From key meta-analysis studies, persons with untreated periodontal infections have up to a 20% increase in their risk of coronary vascular disease1. The multiple of risk for stroke (1.74-2.85 fold) and peripheral vascular disease (1.41-2.27 fold) is equal or greater1. More specifically, the risk of a first myocardial infarction is associated with periodontal disease (OR of 1.49) even after adjustment for a history of smoking, obesity, diabetes and selected socioeconomic factors2. But equally important is the concern for specific bacteria that are a basis for this risk including A.a., P.g., T.f., T.d., F.n. and P.i.3-7. Specifically, Fn carries a series of virulence factors that can contribute to inflammation of the arterial wall8. Toward the interest to prevent heart and vascular disease, testing your patients for which types and what levels of these dangerous bacteria are present will provide them better care.
Metabolic health and Diabetes: ![]()
![]()
![]()
![]()
![]() Elevated levels of periodontal bacteria can directly cause hyperglycemia9. Long term, the inflammation associated with increased pathogen burden can affect the health of the pancreas, and specifically, there is the risk of the loss of beta cells that produce insulin and respond to elevated blood glucose10. Correspondingly, persons with elevated blood glucose are at risk for progressive periodontal infection and inflammation11. So, by these opposing mechanisms, the relationship of periodontal disease and pre-diabetes and diabetes is viewed as a two- way street12. Early detection of periodontal infection and proactive management to reduce bacterial loads can improve blood sugar control and lessen the complications of diabetes as well as the consequence of periodontitis13.
Elevated levels of periodontal bacteria can directly cause hyperglycemia9. Long term, the inflammation associated with increased pathogen burden can affect the health of the pancreas, and specifically, there is the risk of the loss of beta cells that produce insulin and respond to elevated blood glucose10. Correspondingly, persons with elevated blood glucose are at risk for progressive periodontal infection and inflammation11. So, by these opposing mechanisms, the relationship of periodontal disease and pre-diabetes and diabetes is viewed as a two- way street12. Early detection of periodontal infection and proactive management to reduce bacterial loads can improve blood sugar control and lessen the complications of diabetes as well as the consequence of periodontitis13.
Health During Pregnancy: ![]()
![]()
![]()
![]()
![]()
![]() The oral microbiota changes when women become pregnant, and levels of periodontal pathogens increase14. During pregnancy, periodontal inflammation worsens, mostly due to increased levels of A.a., P.g., F.n. and P.i.15. Among these oral pathogens, there is a marked risk of infection of the maternal blood and the placenta, which leads to an increase in pre-term labor, lower birth weight and even the chance of fetal loss due specifically to the bacteria P.g. and F.n. 16,17. Further, the long-term risk for systemic disease in mothers with periodontitis is evident in the progression of atherosclerosis and the increased risk of venous thrombosis due to F.n., P.g., T.f. and A.a.16,18. For these reasons, consider testing all women who are planning a pregnancy with the goal of reducing these bad bacteria.
The oral microbiota changes when women become pregnant, and levels of periodontal pathogens increase14. During pregnancy, periodontal inflammation worsens, mostly due to increased levels of A.a., P.g., F.n. and P.i.15. Among these oral pathogens, there is a marked risk of infection of the maternal blood and the placenta, which leads to an increase in pre-term labor, lower birth weight and even the chance of fetal loss due specifically to the bacteria P.g. and F.n. 16,17. Further, the long-term risk for systemic disease in mothers with periodontitis is evident in the progression of atherosclerosis and the increased risk of venous thrombosis due to F.n., P.g., T.f. and A.a.16,18. For these reasons, consider testing all women who are planning a pregnancy with the goal of reducing these bad bacteria.
Development of Cancer and Risk of Progression: ![]()
![]()
![]()
![]()
![]() Advanced periodontal disease is associated with a 2.5 fold increase in smoking related cancers19. Breast cancer is common, and persons with elevated levels of the bacteria A.a. and P.g. have a greater chance of recurrence or failed response to treatment. In another prospective study, persons with periodontal P.g. showed a 59% increased risk of pancreatic cancer. There are also reports of oral A.a. and T.d. linked to pancreatic tumors20. P.g., T.d. and T.f. are also linked to risk of esophageal cancers21,22. Reducing your patient’s risk of developing cancer by treating periodontal infection is another reason to visit your dentist and request a MyPerioPath® test. A role for the oral bacteria Fn in the progression of colorectal cancer is provocative. Several recent studies show that F.n. can be identified within the primary cancer cells from colonic tumors, and are carried to metastatic sites involving regional lymph nodes23,24. This is a newly observed phenomenon that will affect how cancer treatment protocols will be developed in the future.
Advanced periodontal disease is associated with a 2.5 fold increase in smoking related cancers19. Breast cancer is common, and persons with elevated levels of the bacteria A.a. and P.g. have a greater chance of recurrence or failed response to treatment. In another prospective study, persons with periodontal P.g. showed a 59% increased risk of pancreatic cancer. There are also reports of oral A.a. and T.d. linked to pancreatic tumors20. P.g., T.d. and T.f. are also linked to risk of esophageal cancers21,22. Reducing your patient’s risk of developing cancer by treating periodontal infection is another reason to visit your dentist and request a MyPerioPath® test. A role for the oral bacteria Fn in the progression of colorectal cancer is provocative. Several recent studies show that F.n. can be identified within the primary cancer cells from colonic tumors, and are carried to metastatic sites involving regional lymph nodes23,24. This is a newly observed phenomenon that will affect how cancer treatment protocols will be developed in the future.
Joint and Musculoskeletal Health: ![]()
![]()
![]() Rheumatoid arthritis is a chronic inflammatory condition. In a recent meta-analysis of 21 separate studies, there was a significantly increased risk of periodontitis in people with RA compared to healthy controls (relative risk: 1.13; 95% CI: 1.04, 1.23; p = 0.006; N = 153,277)25. The most prevalent pathogens found were P.g. and F.n. Importantly, the infection and the antibodies against these bacteria are typically found before the onset of symptoms26. The good news is that therapeutic reduction of bacterial load, as determined by molecular tests such as MyPerioPath®, may reduce symptoms and improve the prognosis of the arthritis27.
Rheumatoid arthritis is a chronic inflammatory condition. In a recent meta-analysis of 21 separate studies, there was a significantly increased risk of periodontitis in people with RA compared to healthy controls (relative risk: 1.13; 95% CI: 1.04, 1.23; p = 0.006; N = 153,277)25. The most prevalent pathogens found were P.g. and F.n. Importantly, the infection and the antibodies against these bacteria are typically found before the onset of symptoms26. The good news is that therapeutic reduction of bacterial load, as determined by molecular tests such as MyPerioPath®, may reduce symptoms and improve the prognosis of the arthritis27.
Dementia and Brain Health: Recent medical studies point to poor oral health, and high levels of the bacteria ![]()
![]()
![]() in our gums with the increased risk to develop Alzheimer’s and other types of dementia28-30. Specifically, there is now evidence of P.g present in brain tissue and cerebrospinal fluid may be involved in the production of the abnormal proteins that are characteristic of Alzheimer’s disease31. Additionally, the direct effects of those oral bacteria to cause atherosclerosis in the vessels within the brain impart significant risk for stroke and vascular types of dementia.32
in our gums with the increased risk to develop Alzheimer’s and other types of dementia28-30. Specifically, there is now evidence of P.g present in brain tissue and cerebrospinal fluid may be involved in the production of the abnormal proteins that are characteristic of Alzheimer’s disease31. Additionally, the direct effects of those oral bacteria to cause atherosclerosis in the vessels within the brain impart significant risk for stroke and vascular types of dementia.32
Periodontal Bacteria Measured by the MyPerioPath® Test
| Red Complex Pathogens |
| Actinobacillus actinomycetemcomitans
|
| Porphyromonas gingivalis
|
| Tanerella forsythia
|
| Treponema denticola
|
| Orange Complex Pathogens |
| Eubacterium nodatum
|
| Prevotella intermedia
|
| Peptostreptococcus micros
|
| Fusobacterium nucleatum/periodontium
|
| Campylobacter rectus
|
| Green Complex Pathogens |
| Eikenella corrodens
|
| Capnocytophaga species
|
| Red Complex Pathogens | Orange Complex Pathogens | Green Complex Pathogens |
| Actinobacillus actinomycetemcomitans
| Eubacterium nodatum
| Eikenella corrodens
|
| Porphyromonas gingivalis
| Prevotella intermedia
| Capnocytophaga species
|
| Tanerella forsythia
| Peptostreptococcus micros
| |
| Treponema denticola
| Fusobacterium nucleatum/periodontium
| |
| Campylobacter rectus
|
References
- Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med 2004;15:403-13.
- Ryden L, Buhlin K, Ekstrand E, et al. Periodontitis Increases the Risk of a First Myocardial Infarction: A Report From the PAROKRANK Study. Circulation 2016;133:576-83.
- Pucar A, Milasin J, Lekovic V, et al. Correlation between atherosclerosis and periodontal putative pathogenic bacterial infections in coronary and internal mammary arteries. J Periodontol 2007;78:677-82.
- Radwan-Oczko M, Jaworski A, Dus I, Plonek T, Szulc M, Kustrzycki W. Porphyromonas gingivalis in periodontal pockets and heart valves. Virulence 2014;5:575-80.
- Range H, Labreuche J, Louedec L, et al. Periodontal bacteria in human carotid atherothrombosis as a potential trigger for neutrophil activation. Atherosclerosis 2014;236:448-55.
- Rath SK, Mukherjee M, Kaushik R, Sen S, Kumar M. Periodontal pathogens in atheromatous plaque. Indian J Pathol Microbiol 2014;57:259-64.
- Bale BF, Doneen AL, Vigerust DJ. High-risk periodontal pathogens contribute to the pathogenesis of atherosclerosis. Postgrad Med J 2017;93:215-20.
- Liljestrand JM, Paju S, Pietiainen M, et al. Immunologic burden links periodontitis to acute coronary syndrome. Atherosclerosis 2018;268:177-84.
- Stanko P, Izakovicova Holla L. Bidirectional association between diabetes mellitus and inflammatory periodontal disease. A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2014;158:35-8.
- Janket SJ, Javaheri H, Ackerson LK, Ayilavarapu S, Meurman JH. Oral Infections, Metabolic Inflammation, Genetics, and Cardiometabolic Diseases. J Dent Res 2015.
- Kumar M, Mishra L, Mohanty R, Nayak R. "Diabetes and gum disease: the diabolic duo". Diabetes Metab Syndr 2014;8:255-8.
- Chee B, Park B, Bartold PM. Periodontitis and type II diabetes: a two-way relationship. Int J Evid Based Healthc 2013;11:317-29.
- Kaye EK, Chen N, Cabral HJ, Vokonas P, Garcia RI. Metabolic Syndrome and Periodontal Disease Progression in Men. J Dent Res 2016;95:822-8.
- Persson GR, Hitti J, Paul K, et al. Tannerella forsythia and Pseudomonas aeruginosa in subgingival bacterial samples from parous women. J Periodontol 2008;79:508-16.
- Carrillo-de-Albornoz A, Figuero E, Herrera D, Bascones-Martinez A. Gingival changes during pregnancy: II. Influence of hormonal variations on the subgingival biofilm. J Clin Periodontol 2010;37:230-40.
- Han YW, Houcken W, Loos BG, Schenkein HA, Tezal M. Periodontal disease, atherosclerosis, adverse pregnancy outcomes, and head-and-neck cancer. Adv Dent Res 2014;26:47-55.
- Andonova I, Iliev V, Zivkovic N, Susic E, Bego I, Kotevska V. Can oral anaerobic bacteria cause adverse pregnancy outcomes? Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2015;36:137-43.
- Kurita-Ochiai T, Yamamoto M. Periodontal pathogens and atherosclerosis: implications of inflammation and oxidative modification of LDL. Biomed Res Int 2014;2014:595981.
- Zeng XT, Xia LY, Zhang YG, Li S, Leng WD, Kwong JS. Periodontal Disease and Incident Lung Cancer Risk: A Meta-Analysis of Cohort Studies. J Periodontol 2016:1-13.
- Jacob JA. Study Links Periodontal Disease Bacteria to Pancreatic Cancer Risk. JAMA 2016;315:2653-4.
- Nieminen MT, Listyarifah D, Hagstrom J, et al. Treponema denticola chymotrypsin-like proteinase may contribute to orodigestive carcinogenesis through immunomodulation. Br J Cancer 2018;118:428-34.
- Baba Y, Iwatsuki M, Yoshida N, Watanabe M, Baba H. Review of the gut microbiome and esophageal cancer: Pathogenesis and potential clinical implications. Ann Gastroenterol Surg 2017;1:99-104.
- Amitay EL, Werner S, Vital M, et al. Fusobacterium and colorectal cancer: causal factor or passenger? Results from a large colorectal cancer screening study. Carcinogenesis 2017;38:781-8.
- Yamamura K, Baba Y, Nakagawa S, et al. Human Microbiome Fusobacterium Nucleatum in Esophageal Cancer Tissue Is Associated with Prognosis. Clin Cancer Res 2016;22:5574-81.
- Fuggle NR, Smith TO, Kaul A, Sofat N. Hand to Mouth: A Systematic Review and Meta-Analysis of the Association between Rheumatoid Arthritis and Periodontitis. Front Immunol 2016;7:80.
- Johansson L, Sherina N, Kharlamova N, et al. Concentration of antibodies against Porphyromonas gingivalis is increased before the onset of symptoms of rheumatoid arthritis. Arthritis Res Ther 2016;18:201.
- Khare N, Vanza B, Sagar D, Saurav K, Chauhan R, Mishra S. Nonsurgical Periodontal Therapy decreases the Severity of Rheumatoid Arthritis: A Case-control Study. J Contemp Dent Pract 2016;17:484-8.
- Abbayya K, Puthanakar NY, Naduwinmani S, Chidambar YS. Association between Periodontitis and Alzheimer's Disease. N Am J Med Sci 2015;7:241-6.
- Cerajewska TL, Davies M, West NX. Periodontitis: a potential risk factor for Alzheimer's disease. Br Dent J 2015;218:29-34.
- Pritchard AB, Crean S, Olsen I, Singhrao SK. Periodontitis, Microbiomes and their Role in Alzheimer's Disease. Front Aging Neurosci 2017;9:336.
- Dominy SS, Lynch C, Ermini F, et al. Porphyromonas gingivalis in Alzheimer's disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv 2019;5:eaau3333.
- Choi S, Kim K, Chang J, et al. Association of Chronic Periodontitis on Alzheimer's Disease or Vascular Dementia. J Am Geriatr Soc 2019.