Diabetes
![Thumbnail [200x250]](img/case-study/brie_eickhoff/eickhoff_main.jpeg)
Active Periodontal Disease with Multiple Medical Complications
The Challenge:
A patient with Multiple Sclerosis (MS) and active periodontal disease, was recently diagnosed with type 2 diabetes, will receive periodontal therapy. Currently, proper home care is limited due to the physical difficulties of MS.
The Background:
- Age: 58
- Sex: Female
- Medical History: Several years of MS led to partial left-side paralysis and the inability to use her left hand. To manage type 2 diabetes, metformin was added to a long list of medications which contributed to xerostomia.
- Chief Complaint: Xerostomia, physical difficulties challenging proper home care regimen
- Periodontal Assessment: Generalized 4-5mm edematous pocketing with generalized hemorrhaging
The Solution:
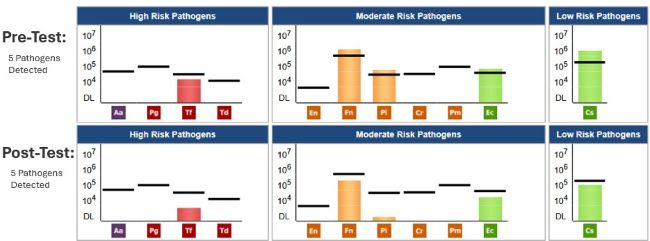
- Date of MyPerioPath® (Pre-Therapy) and OraRisk® Candida Tests: 4/17/2018
- Periodontal Therapy: Biofilm disruption via ultrasonic and laser. Ozone oil therapy applied. Due to the lack of dexterity, PerioProtect™ trays were fabricated and to be worn for 15 minutes 2 times daily.
- Systemic Antibiotic Used: Amoxicillin 500 mg tid for 10 days and Metronidazole 500 mg bid for 10 days
- Home Care: Sonicare with a peroxide and baking soda paste, ProBiora® oral probiotic and CloSYS® Silver mouthwash
- Date of MyPerioProgress® (Post-Therapy) Test: 7/13/2018
The Result:
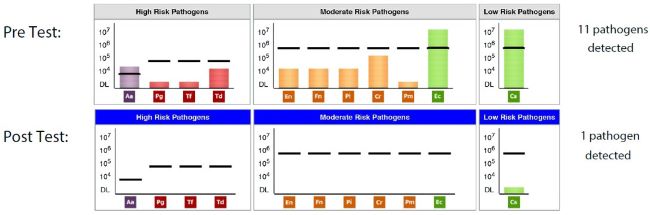
The patient reported using the PerioProtect trays daily along with the other home care changes of an electric toothbrush and localized probiotics. Upon periodontal assessment, complete pocket reduction to healthier levels was noted with no bleeding. The clinical endpoint of absolute clinical sign reduction was complemented by a MyPerioProgress revealing all pathogens below the reference lines, a microbiological endpoint. Patient was placed on a 3-month recall. After a total of 9 months of periodontal maintenance, the patient announced she was no longer on metformin and her A1C levels were completely normal. Periodontally, the patient remained stable. The patient is very satisfied with the results that we as a team were able to accomplish.
About the Author:

Brie graduated from Western Washington University with a bachelors focused on Political Science and Sociology. Having grown up with her dad being a dentist and working in his office she felt compelled to explore the dental field. She moved to New York and completed an AAS in Dental Hygiene at SUNY Binghamton. She has been practicing dental hygiene for over 15 years. She has spent most of her career specializing in the treatment and rehabilitation of periodontal disease.
Brie has attended many courses and received several certifications in the different modes of treatment of periodontal conditions to be able to provide the most effective top-notch care.
Brie has attended several Bale/Doneen preceptorship courses and is listed as a provider for the prevention of Heart Attack, Stroke and Diabetes prevention program. Brie is a member of the American Academy of Oral Systemic Health. She focuses treatment around patients’ oral systemic health. This approach allows her to evaluate oral/systemic health based on lifestyle, diet, medications, systemic conditions, oral periodontal pathogens present in mouth tested via saliva sampling, inflammatory bloodwork, sleep patterns, and airway evaluation.
The modes of treatment Brie is trained and extremely experienced in allow her to provide the most optimal care to her patients. She is certified in laser assisted periodontal therapy, the use of an endoscope, supportive bone regenerating biological proteins, and individualized home maintenance care.
![Thumbnail [200x250]](img/case-study/Carter%20Lamb%20RDH%20Case%20Study_162149746.jpg)
Periodontal Patient with Poor Diabetic Control Combined with Poor Home Care
The Challenge:
A periodontal patient of record is diagnosed with active periodontal disease. Therapy is needed to achieve a healthier oral state; however, the patient has uncontrolled diabetes and poor home care that may be contributing to the patient’s oral health status.
The Background:
- Age: 48
- Sex: Female
- Medical History: Diabetes, high blood pressure, high cholesterol, thyroid disease
- Last Dental Exam: 3/6/19
- Home Care: Not very diligent with homecare. Has PerioProtect™ trays but does not use them regularly. Uses Peridex™ daily. Patient does not floss regularly.
- Chief Complaint: Bleeding gums
- Other Notes: Blood sugars very high
- Clinical Assessment: Inflammation with bleeding, moderate calculus build up.
- Periodontal Assessment: Generalized 4-6mm pockets with bleeding on probing.
- Medical Assessment: Uncontrolled diabetes
The Solution:
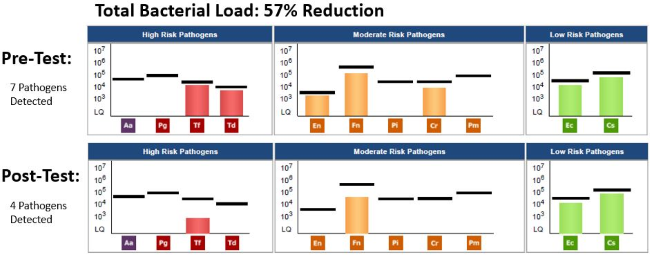
- Date of Pre MyPerioPath® (pre-therapy test): 11/19/2018
- Periodontal Therapy: Scaling and root planing
- Medical Therapy: Patient has nutritionist and diabetes counselor.
- Systemic Antibiotic Use: Doxycycline 100 mg bid for 8 days
- Home Care Instruction: PerioProtect trays, Peridex, CoQ10 and Vitamin D
- Date of MyPerioProgress® (post-therapy test): 1/24/2019
Additional comments: The Systemic Effects of Oral Pathogens, page two of the MyPerioPath report helped in educating the patient that there were several bacteria that could be complicating her diabetic control.
The Result:
After therapy and a period of time for healing, the MyPerioProgress post-therapy specimen was collected on 1/24/2019. Upon periodontal evaluation after therapy, the tissue appeared to be healthier. There was a dramatic reduction of calculus and decrease in bleeding on probing. The patient’s overall skin appearance was improved and she indicated better control of her blood sugars.
I learned that we need to use OralDNA tests more often, so we can have an objective measurement of what the therapy achieved. The patient appreciated seeing the more dramatic changes in the biofilm. She realizes her periodontal status is delicate and it can impact her overall health. We will continue to monitor her compliance and administer another MyPerioPath when her disease state relapses.
About the Author:

Carter joined the Dycus Dental team in 2018. She graduated from Tennessee State University in 2015 and served as the class secretary. She moved to Cookeville in 2018 from Macon, Georgia.
Carter loves her coworkers and the family atmosphere at our office. She enjoys giving specific care to each of our patients and has a positive attitude and a smile on her face every day!
Carter married her husband Tre in 2015. When she is not at the office she enjoys traveling, exercising, reading and watching Tennessee Tech football games.
![Thumbnail [200x250]](img/case-study/Diabetes%20Case%20Study_178569825.jpg)
Type II Diabetic and Periodontal Disease
The Challenge:
A Type II Diabetic patient, who has been a long term client, has uncontrolled periodontal disease and a history of not responding to previous periodontal treatment.
The Background:
- Age: 73
- Sex: F
- Medical History: Type 2 Diabetes, gout, high blood pressure, kidney issues
- Last Dental Exam: Sept 2017
- Home Care: Patient has been on periodontal maintenance regimen
- Chief Complaint: Bleeding gums, high blood glucose, overall in poor health and not feeling well
- Other Notes: Nutritional - Patient states she is trying to control blood sugars, but they have been out of control
- Clinical Assessment: Bleeding gums, advanced periodontal disease around #2, unopposed 7-8mm pocketing
- Periodontal Assessment: Advanced periodontal disease
- Medical Assessment: Uncontrolled diabetes
The Solution:
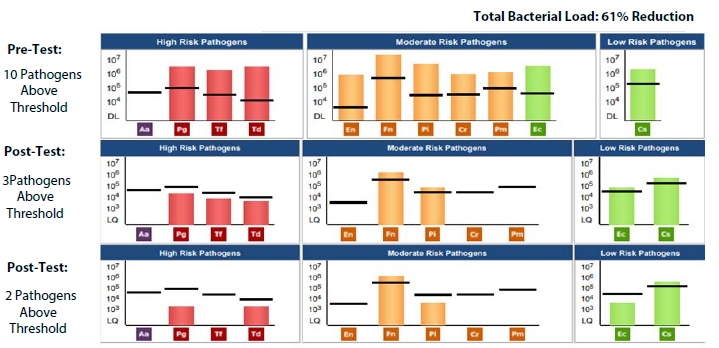
- Date of Pre-MyPerioPath® (pre-therapy test): 1/11/2018
- Periodontal Therapy: Extraction #2, 4 quads of scaling and root planing, air flow polisher with glycine powder for biofilm reduction
- Medical Therapy: Ongoing with primary physician
- Systemic Antibiotic Use: Amoxicillin 500mg tid for 8-10 days AND Metronidazole 500mg bid for 8-10 days, depending on the severity of infection.
- Home Care: ProBiora® Pro-oral probiotics, Immune tabs from Hyperbiotics®, Sonicare toothbrush
- Other Notes: Patient declined Perioscience® product.
- Date of MyPerioProgress® (post-therapy test): 4/17/2018 and 9/8/2018
Additional comments: Patient declined 3rd script of Metronidazole and Amoxicillin. Patient to continue with ProBiora Pro oral probiotics, Immune tabs and Sonicare usage as well as an improved diet and exercise routine. Patient has an appointment with her nephrologist soon and will consult on antibiotic usage. Patient will probably wait for 6 months for her next saliva test. Pt is very pleased with her results and how her general health has improved.
The Result:
At the 3 month evaluation including a MyPerioProgress the patient had improved but periodontal concerns still remained. A second round of systemic antibiotic was administered based on the second MyPerioPath results and a follow-up was scheduled. Following the second MyPerioProgress - total of three MyPerioPath tests performed 9 months after therapy, a 61% reduction of the total bacterial load was achieved. The patient is very pleased with her periodontal results and feels the zinc supplements have helped the blood sugar control. We have helped her achieve good periodontal health while helping her decrease health risks. Medically, the patient has seen great improvements. Her blood sugar is now 100-120 and she is working with her medical team to lower or eliminate some of her diabetic medicines. “The saliva testing has given us a great way to add science to the equations and give us quantitative results.”
About the Author:

![Thumbnail [200x250]](img/case-study/Uncontrolled%20Diabetic-%20Referred%20by%20Physician%20Case%20Study_153024675.jpg)
Uncontrolled Diabetic- Referred by Physician
The Challenge:
To find the source of her inflammation and infection. If the source is of a bacterial nature, then the goal is to reduce the bacteria. By reducing the bacterial load, the hope is to reduce or eliminate medications for diabetes and blood pressure. Please note: The patient accepts her responsibility for the decline in her overall health.
The Background:
- Age: 41
- Sex: Female
- Medical History: Type II Diabetes, High BP, acid reflux
- Family History: Cardiovascular disease, diabetes and cancer
- Last Dental Exam: 2008
- Home Care: Manual toothbrush
- Chief Complaint: “My doctor said my uncontrolled diabetes could be caused by my mouth.”
- Other Notes: Soda consumption
- Clinical Assessment: Sub-gingival and supra-gingival calculus present, tissue inflamed and bulbous
- Periodontal Assessment: Localized chronic, active periodontal disease, slight to moderate
The Solution:
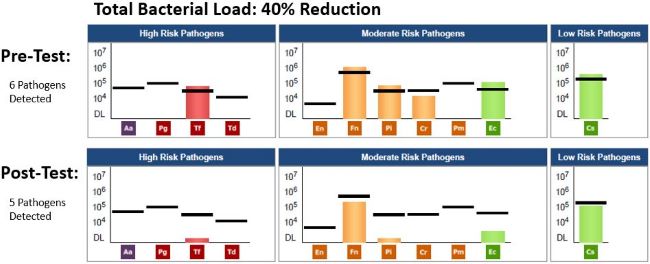
- Date of Pre MyPerioPath® (pre-therapy test): 7/27/2017
- Periodontal therapy: Level 5 Full mouth therapy performed. The “5 tip” cavitron method was incorporated with irrigation of water and chlorhexidine. Arestin® was placed in pockets 5mm or greater.
- Systemic Antibiotic Used: As indicated by the MyPerioPath results
- Home Care: Sonicare toothbrush, Waterpik™, ProBiora® Pro-Dental Probiotic and Periosciences® A.O Gel
- Other Notes: Patient was placed on strict home care routine
- Date of MyPerioProgress® (post-therapy test): 10/19/2018
The Result:
Post therapy results were exciting for both the patient and myself. A major biofilm shift was noted with the reduction of the bacteria responsible for her inflammation. Reduction of pocket depth, bleeding and inflammation was noted. The patient was able to discontinue use of three diabetic medications, preventing the need for diabetic injections! The patient also stated losing 20 lbs., which has stabilized her blood pressure, and reported a pleasant reduction of acid reflux. My patient was thrilled with the overall results and has noticed a huge difference with the way her mouth looks and feels. Reflecting on this case, it is imperative to have all the information on which bacteria are causing the problem. Having the evidence, allows the clinician to tailor the treatment for each patient in order to target the cause and measure the effectiveness following treatment.
About the Author:

![Thumbnail [200x250]](img/case-study/Dental%20Hygienist%20with%20Type%20II%20Diabetes%20Case%20Study_113201522.jpeg)
Dental Hygienist with Type II Diabetes
The Challenge:
Knowing the scientific information that clearly confirms the bi-directional relationship with diabetes and periodontal disease, our goal is reduce the periodontal pathogens to improve the diabetic status.
The Background:
- Age: 38
- Sex: F
- Medical History: Recently diagnosed with Type II Diabetes. See Nutrition Notes.
- Family History: Type II Diabetes & Periodontal Disease
- Last Dental Exam: 8 weeks ago
- Home Care: Meticulous consisting of electric toothbrush 2x/day, flossing daily and waterpiking 1x/day
- Nutrition Notes: Her physician agreed to her commitment to diet and lifestyle changes before considering medication to control her diabetes. These changes included regular exercise and eliminating sugar.
- Chief Complaint: “When it comes to my diabetes, I know what to do, I just have to do it!” Also, the patient is a dental hygienist, she wants to know she is doing everything possible orally.
- Periodontal Assessment: No bleeding on probing, scattered 4mm posterior areas of 1 mm recession, no visible inflammation and excellent plaque control. Grayish tissue color (most likely due to lack of circulation) with lack of stippling around crowns. Residual light calculus around crown margins. Radiographic evidence of posterior bone loss.
The Solution:
- Date of Pre-MyPerioPath® (pre-therapy test): 9/10/2015
- Periodontal therapy: Removal of residual marginal calculus around crowns and complete biofilm disruption with ultrasonic slim line inserts, hand scaling with curettes and subgingival airpolish conducted in two appointments.
- Systemic Antibiotic Used: No systemic antibiotics were administered due to patient wanting to see what her body could do first.
- Lifestyle & Diet changes
- Home Care: Remained the same
- Date of MyPerioProgress® (post-therapy test): 3/10/2016
The Result:
The periodontal changes were favorable; the color and texture of tissue presented healthy and the 4 mm pockets reduced to 3mm. The MyPerioPath® post-therapy results (MyPerioProgress®) showed a dramatic shift in the bacterial load. More importantly, when the patient presented to her medical doctor to evaluate her diabetic control, she had reversed her diagnosis. Her lab tests confirmed a normal A1C and blood glucose levels.
This patient is most grateful that she had the opportunity to test for periodontal pathogens and had a relatively simple treatment to eliminate the pathogens and positively influence her diabetic diagnosis! This case highlights the role of dental care with overall health, the need to comanage patients and the need for patient cooperation.
About the Author:
