Periodontitis
![Thumbnail [200x250]](img/case-study/carey_duraiappa/duraiappa_main.jpeg)
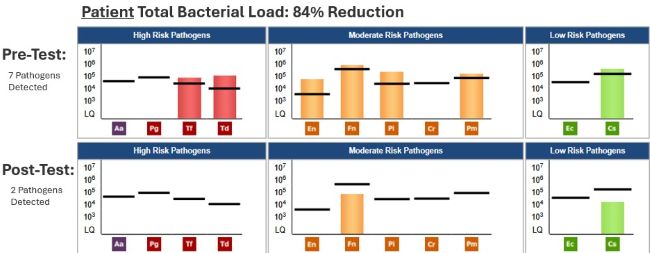
Transmissible Bacteria Between Spouses
The Challenge:
My patient was very concerned about passing bacteria to his wife and young daughter.
The Background:
The patient knew he had periodontal issues and was informed that he would likely need to see a periodontist.
Patient:
- Age: 36
- Sex: M
- Medical History: Essential hypertension
- Last Dental Exam: 6 months to a year
- Home Care: Good home care
- Chief Complaint: Needs cleaning
- Other Notes: Reports increased stress over last year.
- Periodontal Assessment: Stage II & III, Grade B, generalized calculus noted on bitewing x-rays, moderate bleeding and inflammation.
Spouse:
- Age: 32
- Sex: F
- Last Dental Exam: 6 months
- Home Care: Fair
- Chief Complaint: None; “wants cleaning,” concerned about saliva test due to husband’s results.
- Clinical Assessment: Localized 4mm pockets, generalized mild inflammation, localized moderate subgingival calculus.
- Periodontal Assessment: Stage I, Grade B
The Solution:
Patient Solution:
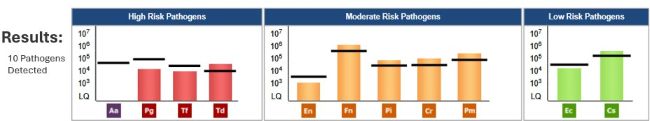
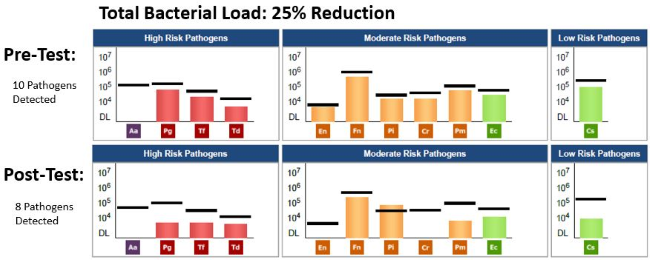
- Date of OralDNA® (Pre-Therapy) tests: Alert 2™ 07/22/2022
- Periodontal Therapy: Scaling and root planing all quadrants, laser, irrigation
- Systemic Antibiotic Used: Amoxicillin 500 TID and Metronidazole 500 BID
- Home Care: Recommended using an electric toothbrush, floss and proxybrush.
- Other Notes: Periodontal maintenance visit (PMV) with laser and irrigation on a 3-month interval.
- Date of MyPerioProgress® (Post-Therapy) Test: 09/14/2022
Spouse Solution:
- Date of Alert 2™ (Pre-Therapy) test: 08/09/2022
- Periodontal Therapy: Prophylaxis
- Systemic Antibiotic Used: None
- Home Care: Recommended using an electric toothbrush and string floss instead of floss picks
- Date of MyPerioProgress(R) (Post-Therapy) Test: 08/10/2023
The Result:
I learned certain bacteria are highly transmissible. Their tests were almost identical following my patient’s therapy. Her clinical signs did increase over the year even though her bacterial levels decreased resulting in her need to have periodontal therapy. Her bacteria reduced by 82% and left her with only 2 bacteria to her husband’s past results indicating her disease state may be due to another cause.
This is good insight for patients who had clinical improvements, but their bacteria do not reduce. Also, I am more aware and ask, “Do you know the periodontal health of your spouse/significant other/etc..?” because both of the patients’ MyPerioProgress tests were almost identical even though they were a year apart and had different therapy completed.
About the Author:
Carey has been a dental hygienist for 25 years and while she has practiced clinical dental hygiene the entire time, she also has 12 years of experience in practice management. However, her heart has always been with direct patient care. Carey has been with Pacific Dental Services for nearly 2 years now and feels very fortunate to be with a company who truly cares about and understands the mouth body connection. Being able to offer saliva testing has been a game changer for her and her patients. Carey states: “There are really two enemies in periodontal disease, the bacteria and our body's response to it. We are so fortunate to have a test that will tell us both of those things. It also makes it so much more relatable to the patient, and they can see their progress.”
Carey likes to spend her spare time with her family, especially her children. Her oldest daughter, Savanna, teaches animal science in Lamar, Colorado. Her husband, Skyler, is a cattle rancher, and they are expecting their first child in January. Carey’s daughter, Isabelle, just graduated from NDSCS, Carey's alma mater, and is working as an RN for Sanford in Fargo, ND. Her son Lucca is 14 and in his first year of high school. He joined the marching band this year and enjoys sailing and golf in the summer. Carey’s youngest son, Aiden, is 13 and in his last year of middle school. Golf is his passion, and he would love to do that every day of the year.
![Thumbnail [200x250]](img/case-study/jennifer_campbell/campbell_main.jpeg)
Testing & Treatment When the Timing is Right
The Challenge:
A patient of record since 2014, single dad and full-time factory plant worker came in for a routine dental.
The Background:
- Age: 33 years old
- Sex: Male
- Medical History: Asthma, high blood pressure, patient has history of smoking, on and off up to a pack per day.
- Last Dental Exam: 2020
- Home Care: Brush, floss, rinse, shower flossing device
- Clinical Assessment: Dental history shows high caries risk, and adult periodontitis. The patient shows current clinical evidence of uncontrolled periodontal disease, not responsive to traditional therapy (cleaning and homecare).
- Medical Assessment: Current medications are Rosuvastatin, Lamictal®, Lisinopril and Oxybutynin.
Additional Information: In 2014, a recommendation for testing was declined because he did not feel he could afford it at that time. Today the timing was right.
The Solution:
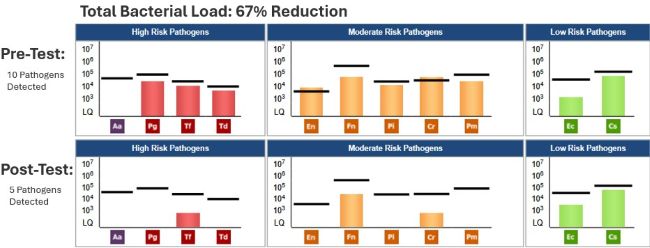
- Date of MyPerioPath® (Pre-Therapy) Test: 01/14/2021
- Dental/Periodontal Therapy: Scaling and root planing (SRP) with anesthetic, piezo removal of hard, soft and bacterial deposits, manual hand scaling and air polishing.
- Systemic Antibiotic Used: Amoxicillin and Metronidazole
- Home Care: Continue existing protocol.
- Other Notes: Recommendation is 3 month follow up care appointment.
- Date of MyPerioProgress® (Post-Therapy) test: 07/21/2021
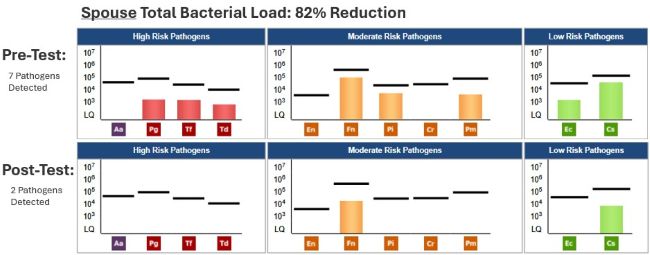
The Result:
This patient had an excellent response to SRP and antibiotic therapy with a bacteria load decrease of 65%. Patient is more consistent with a good oral care routine and cleaning his mouth more often.
About the Author:
Jennifer is a dental hygienist with over a decade of experience working in private and public health dentistry. Outside of work, she enjoys spending time with her family.
![Thumbnail [200x250]](img/case-study/chelsea_gonzales/gonzales_main.jpeg)
Neglected Active Periodontal Disease
The Challenge:
A new patient, a 59-year-old male, presents to our office with no specific concerns. However, a previous provider recommended a “deep cleaning.” This “deep cleaning” treatment was never completed. Patient has 4 fully erupted wisdom teeth that are difficult to access for daily cleaning.
The Background:
- Age: 59
- Sex: Male
- Medical History: High Blood Pressure but is taking medication
- Last Dental Exam: 2019
- Home Care: Manual toothbrush 2x daily, baking soda with peroxide, floss occasionally
- Chief Complaint: None
- Clinical assessment: Severe gingival inflammation, moderate plaque with heavy calculus sub/supragingival. Moderate to severe bone loss is evident on radiographs
- Periodontal Assessment: 2-9mm pocketing, Class I furcations noted, localized bone loss 15-33%
The Solution:
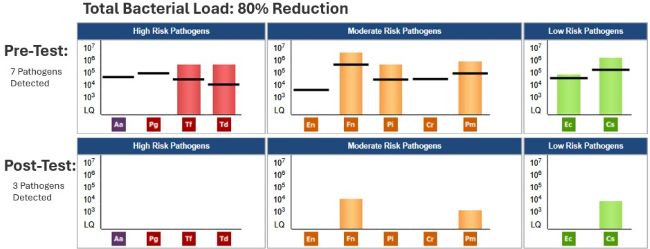
- Date of MyPerioPath® (Pre-Therapy) test: 6/3/21
- 6/4/21: Right side upper & lower scaling & root planing performed with left side irrigation
- 6/8/21: Left side upper & lower scaling & root planing performed with right side irrigation
- Systemic Antibiotic Used: Full mouth irrigation, review of results and prescription for Metronidazole and Amoxicillin on 6/15/21.
- 5/2022: Patient presents for periodontal maintenance, exam, and radiographs
Additional Comments: Patient did finish the prescribed antibiotics however he has not been compliant with flossing or his re-care visits. He stated he thought the Waterpik™ could replace flossing.
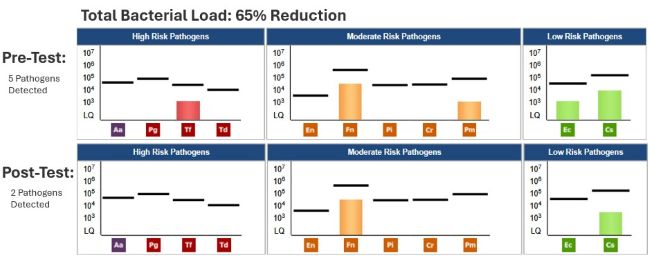
The Result:
At 6 months after completion of the initial scaling & root planing appointments the patient showed improvement in pocket depths and tissue appearance. MyPerioPath® comparison also showed a dramatic reduction in the bacterial load. At his visit a year later, the tissue continues to show health except for around the wisdom teeth. It has been recommended to extract tooth #1 due to decay. We will continue to encourage consistent hygiene appointments, improved home care and bacterial monitoring to help ensure long term remission of the periodontal disease.
About the Author:

Dr. Gonzales is a top 5-Star rated General and Cosmetic dentist who is committed to providing high-quality dental care based on the foundation of honesty. “Honesty guides me at all times because patients trust me with their health. I go home each day feeling good about what I do.”
Dr. Gonzales’s daily inspiration is helping patients believe in their health. “It is a reward to help my patients achieve a comfortable and confident smile. I am just a catalyst, but they are the one who takes ownership, invests in, and maintains their oral health. I am so fortunate to be part of the process.”
She is originally from a small town in Southern California and completed her undergraduate education at University of California, Berkeley. Later she graduated with high honors from University of the Pacific, Arthur A. Dugoni School of Dentistry.
After ten years in San Francisco, Dr. Gonzales moved to Albuquerque to practice with her uncle Dr. Charles Gallagher. “It was an opportunity I could not pass up. Academy Dental Care is an outstanding dental office, as you will soon find out!”
When Dr. Gonzales is not in the office, you can find her on her Pelaton exercise bike! She also likes skiing, tennis, hiking, traveling, and spending time with her family.
![Thumbnail [200x250]](img/case-study/andrea_farago/farago_main.jpeg)
Dental Hygiene Student Helps Manage Periodontal Disease Through MyPerioPath<sup>®</sup> Testing
The Challenge:
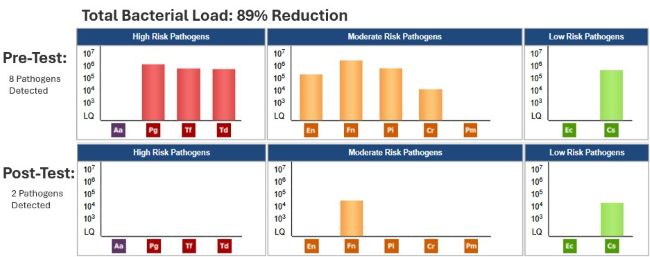
To reduce periodontal pathogens in the oral cavity that are contributing to severe periodontal inflammation and tissue sensitivity.
The Background:
- Age: 33
- Sex: F
- Medical History: History and treatment for ovarian cancer.
- Home Care: Brushing 1x/day and infrequent flossing.
- Periodontal Assessment: Class 1, Stage B with extreme bleeding.
The Solution:
- Date of MyPerioPath(R) (Pre-Therapy) Test: 1/18/2022
- Periodontal therapy: 4 appointments of periodontal debridement with ultrasonics, hand instrumentation, and laser-assisted bacterial reduction therapy.
- Home Care: Proper toothbrushing techniques for twice a day and flossing once a day.
The Result:
A significant decrease in bleeding upon probing was noted already at the first few appointments during treatment. After the patient had received all treatments needed to finish her periodontal therapy, it was riveting to see such drastic improvement. Bleeding upon probing was greatly reduced! The previously inflamed and irritated gingiva was flat and healthy. The patient stated that she has been making sure to brush properly twice daily and floss more frequently. Although it is impossible to remove all bacteria from the mouth, the goal is to find a balance point where the pathogens aren’t causing harm. From the decrease, and in some areas the absence of any clinical signs, we are heading in the right direction to a much healthier overall oral environment.
In summary, it would be beneficial to perform a post-treatment MyPerioPath® analysis along with consistent periodontal maintenance visits for this patient. Overall, this experience with OralDNA® Labs salivary testing was very eye-opening and a fantastic learning opportunity. I hope to be able to use this amazing resource throughout my dental hygiene career. It is a great way to understand and confirm potential causes of oral disease and help to create the best treatment plans for patients.
About the Author:

Andrea Farago graduated from Colorado Northwestern Community College in 2022.
Dental hygiene has always interested her since she was young. Developing personal relationships through real hands-on contact while educating on the importance of good oral health and inspiring them to better their home-care habits will certainly be her passion. During her formal education, she enjoyed participating in community programs and volunteer opportunities planned by the school’s SADHA program.
Andrea has been blessed with a culturally diverse childhood. Originally born in Budapest, Hungary, where most of her family lives, to eleven years in Saudi Arabia to eventually finish her primary education in Bailey, Colorado, a mountain town close to Denver. This allowed her opportunities to travel, experience different cultures and experiences. Traveling the world is a life goal and she plans to share her dental hygiene knowledge everywhere she finds herself.
In her free time, she enjoys doing artsy activities, including drawing, painting, and sculpting. She loves spending time with my friends and family and going on fun adventures with the people she loves.
![Thumbnail [200x250]](img/case-study/monica_vigon/vigon_main.jpeg)
Periodontal Disease with a Patient Experiencing Vision Impairment
The Challenge:
Patient is experiencing recent vision impairment presented as Stage III Grade B, active generalized periodontal disease with localized severe periodontal disease in the maxillary anterior area.
The Background:
- Age: 36
- Sex: M
- Medical History: Patient reports recent vision impairment with the right eye. Under the care of the ophthalmologist, a diagnosis has not been found. No other systemic diseases or conditions reported.
- Last Dental Exam: Within 3 years
- Chief Complaint: Loose anterior tooth with mild discomfort.
- Clinical Assessment: Class III Mobility on teeth 8 and 10, no clinical findings of decay. Patient reports no history of trauma to the head or neck.
- Periodontal Assessment: Generalized 3-5mm probing depth with localized 9+ probing depths on teeth 7 and 8. Generalized bleeding in all 4 quadrants. Suppuration from teeth 8 and 10.
Additional Comments: Patient states he noticed loosening of teeth around same time as vision impairment. This occurred approximately 3 months prior to the dental exam.
The Solution:
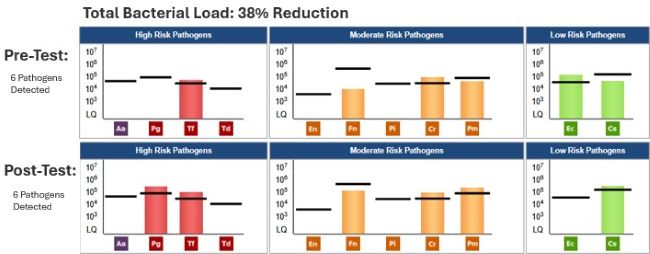
- Date of MyPerioPath® (Pre-Therapy) test: 12/21/2020
- Periodontal Therapy: Full mouth scaling and root planing, irrigation, and bacterial decontamination.
- Systemic Antibiotic used: Metronidazole 500mg 10 days.
- 6 weeks post SRP: Consult with Periodontist and extract teeth 8 and 10.
- Date of MyPerioProgress® (Post-Therapy)Test: 02/18/2021
- 3 months post extract; cone beam computed tomography (CBCT) and evaluation for implants by periodontist. Areas of teeth 8 and 10 showed not enough bone for implant placement. Permanent bridge was recommended and completed for this patient.
Additional comments: During the full course of therapy, the patient discontinued the use of medication for his ophthalmic problems and reported a stabilization on vision loss. The patient’s ophthalmologist requested copies of our salivary diagnostics results to investigate further.
The Result:
There was generalized improvement in all 4 quadrants resulting in 1-3mm probing depths with no bleeding. The microbiological reduction of 67% resulted in his periodontal health. The patient has been able to maintain this periodontal health for one year and counting. The patient has been consistent with our recommendation of a 3-month hygiene care where a periodontal maintenance, irrigation and bacterial decontamination is performed each time.
Although the patient was unable to have implants to replace missing teeth 8 and 10, the fixed bridge #6-#11, along with stabilization of his vision has restored his self-confidence. This case has taught me to be confident with our treatment protocols. Even though this case had a twist–the vision impairment and the recognition of the loose anterior teeth—our treatment protocol had a positive correlation. This case supports the information we currently know about the Mouth Body Connection™ is just the tip of the iceberg.
About the Author:
Dr. Vigon has been practicing dentistry since 2011. She strives to provide painless, pleasant, and beautiful dentistry to all of her patients. She has volunteered with organizations such as Mission of Mercy and Autism Speaks Walk. Aside from providing exceptional dental care, she can be found spending time with her family, friends, and her dog, Lucas. Dr. Vigon enjoys attending the local food, art, and music shows that the beautiful city of Miami has to offer. Her favorite book is Find Your Extraordinary: Dream Bigger, Live Happier, and Achieve Success on Your Own Terms. Her favorite show is Modern Family, and her favorite team is the Miami Heat.
![Thumbnail [200x250]](img/case-study/brenda_sullivan/sullivan_main.jpeg)
Classic Periodontal Disease after COVID
The Challenge:
Patients are avoiding routine dental visits due to fear of contracting COVID. This patient had missed several hygiene appointments during the pandemic. Our goal was to re-establish health and increase home care to help this patient’s general immunity.
The Background:
- Age: 84
- Sex: Male
- Medical History: History of cancer, high cholesterol, arthritis. Medications include Crestor® and fenofibrate. BP: 114/72 P: 83 Temp: 97.3
- Last Dental Exam: 12/02/2020
- Home Care: Poor. Patient was homebound due to the pandemic. Daily brushing stopped and consumption of sweets increased.
- Chief Complaint: Wanted to get his teeth cleaned.
- Clinical Assessment: Missing #1, 2, 15, 16, 17, 30, 31, 32. #12 is an existing implant, #13 broken at gum line, #11 gross decay under gum, furcation involvement with #14, 18, 19 and 3, and generalized mobility.
- Periodontal Assessment: Adult chronic generalized moderate periodontal disease with localized severe periodontal disease.
The Solution:
- Date of MyPerioPath® (Pre-Therapy) Test: 12/02/2020
- Periodontal Therapy: 4 quads of scaling and root planing under Oraqix with ultrasonics, hand instruments and irrigation with diluted betadine.
- Systemic Antibiotic Used: Amoxicillin 500 mg tid for 10 days and Metronidazole 500mg bid for 10 days
- Home Care: Use Oracare medicated mouth rinse 2x/day and oral probiotics, gum line brushing with Sonicare toothbrush and Waterpik™ daily.
- Date of MyPerioProgress® (Post-Therapy) Test: 4/19/2021
The Result:
This pandemic has taken a toll on several of our patients. I am grateful when they return for care even if I expect most to need our help to become healthier. This case study is an example of what can be achieved with the partnership of the patient to provide appropriate home care and personalized periodontal therapy based on clinical lab results from OralDNA® Labs.
About the Author:

Brenda Sullivan is a registered dental hygienist in Austin, TX. She attended the University of Texas Health Science Center where she graduated with a Bachelor of Science in Dental Hygiene in 2004. Brenda has been working at Arbor Oaks Dental with Dr. C. Ian Brawner, DMD since he took over the practice in 2016. The focus at Arbor Oaks Dental is complete and comprehensive care for each patient. Brenda has also trained through the IAOM for Myofunctional Therapy and will be working at IMyo: Orofacial Myology of Central Texas https://imyotherapy.com/.
![Thumbnail [200x250]](img/case-study/pete_williams/williams_main.jpeg)
Periodontal Disease and Rheumatoid Arthritis – Controlling Two Birds with One Stone?
The Challenge:
Our case study represents an example of the emerging evidence from interventional and, more recently, animal studies showing how seemingly unrelated diseases such as periodontal disease and rheumatoid arthritis can be related through similar genetic, biological, and clinically consistent mechanisms.1,2,3,4.
The Background:
- Age: 57 years old
- Sex: F
- Medical History: Diagnosis of Palindromic Rheumatism, elevated hs-CRP 26.2, APOE3/3, stool test indications of possible SIBO, comprehensive testing results revealing Vitamin B concerns.
- Periodontal Assessment: Generalized plaque, high level of bleeding on probing, generalized bone loss of approximately 40% with probe depths ranging from 2mm-7 mm with furcation involvement. Extremely elevated rate of collagen breakdown and high levels of a biomarker activated MMP-8 (43.16 ng/ml). (ideally < 20 ng/ml)
Medical Assessment: The right-side extremities have been impacted with the knee having a large Baker’s Cyst, swollen right ankle with a reduction in feeling in the foot, reduced range of motion overall and stiffness in right wrist and several finger joints in both hands.
The Solution:
- Date of MyPerioPath® (Pre-Therapy) Test: 7/7/2020
- Periodontal Therapy: Guided biofilm therapy every 2-3 months,
- Medical Therapy: Anti-inflammatory focus with curcumin 500 mg bid, Omega 3 oil 2.5g, increase phytochemical density with a variety of real whole food, green tea and collagen.
- Home Care: Re-mineralizing toothpaste and antiseptic mouthwash, TePe™ brushes (interdental), floss twice a day and brush twice a day with an electric toothbrush. A tongue scraper in the evening was introduced.
- Date of MyPerioProgress® (post-therapy test): 9/22/2020 and 11/17/2020
The Result:
At 8 weeks post dental and functional medicine treatment, the patient observed a decrease in swelling and joint soreness, especially in her hands and wrists. Her perception of daily pain significantly reduced. The Baker’s cyst reduced in size approximately 50%. CRP dramatically improved, reducing from 26.2 to 4.8. With the increased bacterial load but reduced disease activity (MMP8 40-MMP8 <10), we theorize that, based on the oral genomic data, more bacterial interventions will continue to calm local and systemic inflammation and modulate acquired immunity, continuing to reduce active periodontal disease and systemic inflammation.
About the Author:

Founder of Functional Medicine Associates, Pete is an exercise and medical scientist. In 2002, he was part of the UK’s founding group of Certified Strength and Conditioning Specialists, as accredited by the National Strength and Conditioning Association of America. In 2004, he became the youngest ever recipient of a ‘Lifetime Achievement’ award from the Register for Exercise Professionals. In 2013, he was in the first worldwide cohort to be awarded the Institute for Functional Medicine Certified Practitioner status and has represented the Institute for Functional Medicine as a Clinical Innovator.
Pete has had over 20 years of experience applying Functional Medicine in clinical practice and is seen by his peers as one of the leading figures in Functional Medicine in the UK. He is a sought-after speaker and advisor to nutraceutical and lab testing companies. Throughout this time, he has treated people with a wide range of chronic diseases.
![Thumbnail [200x250]](img/case-study/brenda_dunlop/dunlop_main.jpeg)
Classic Periodontal Disease
The Challenge:
A new patient with poor home care and lack of dental attention presented wanting whiter teeth along with a cleaning.
The Background:
- Age: 40
- Sex: M
- Medical History: No medical conditions or medications; generally healthy (BP 118/79).
- Last Dental Exam: 3/8/2017
- Chief Complaint: Whiter teeth
- Clinical Assessment: Severe wear on anterior teeth and decay on #19.
- Periodontal Assessment: Adult chronic periodontal disease
Additional Comments: There is a suspicion of sleep disordered breathing along with an anterior tongue tie.
The Solution:
- Date of MyPerioPath® test: 7/22/2020
- Periodontal therapy: 4 quadrants of scaling and root planing(SRP) under Oraqix® with ultrasonics, hand instruments and irrigation with diluted betadine.
- Systemic Antibiotic used: Amoxicillin 500 mg tid for 10 days and Metronidazole 500 mg bid for 10 days was administered immediately following scaling and root planing.
- Home Care: Patient was instructed to use OraCare medicated mouth rinse 2 times/day and oral probiotics, in addition to gumline brushing and Waterpik™ use daily.
- Date of MyPerioProgress® (post-therapy) Test: 10/5/2020
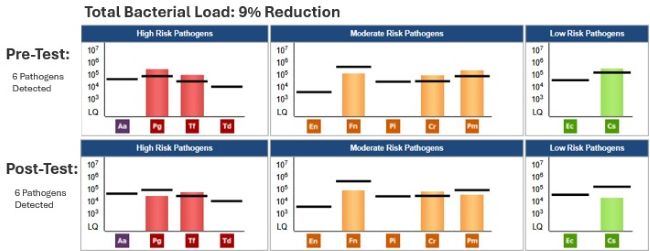
The Result:
The patient responded to the periodontal therapy favorably, resulting in zero bleeding on probing. We will continue to monitor some isolated periodontal pockets on #14DB and #15MB and test again when needed. The post MyPerioPath® had a 70% reduction in periodontal pathogen (burden) load which is a significant shift. Patient was very happy with the look and feel of his teeth. In subsequent visits, we will address our suspicion of sleep disordered breathing.
About the Author:

Brenda Dunlop is a registered dental hygienist in Austin, TX. She attended the University of Texas Health Science Center where she graduated with a Bachelor of Science in Dental Hygiene in 2004. Brenda has been working at Arbor Oaks Dental with Dr. C. Ian Brawner, DMD since he took over the practice in 2016. The focus at Arbor Oaks Dental is complete and comprehensive care for each patient. Brenda has also trained through the IAOM for Myofunctional Therapy and will be working at IMyo: Orofacial Myology of Central Texas https://imyotherapy.com/
![Thumbnail [200x250]](img/case-study/daniela_yanez/yanez_main.jpeg)
Chronic Anterior Inflammation Finally Resolved
The Challenge:
The patient's main concern was to reduce chronic inflammation around tooth #8 and #9. The patient previously had received treatment at a general dentist and a periodontist without significant improvement.
The Background:
- Age: 28
- Sex: F
- Medical History: Patient stated that she is in good overall health.
- Family History: Breast and renal cancer, cardiovascular disease, high blood pressure and heart attack, type 2 diabetes, and Alzheimer’s disease
- Last Dental Exam: 12/05/2018
- Home Care: Brushing twice daily with Tom's of Maine toothpaste and a Sonicare power toothbrush, and Crest® ProHealth™ rinse with occasional flossing.
- Chief Complaint: This area (maxillary anterior) has been addressed by various providers with no improvement.
- Periodontal Assessment: Generalized inflammation and bleeding with 3-6mm periodontal pockets, moderate subgingival calculus, and light generalized plaque. Radiographs revealed horizontal and vertical bone loss while the bacterial slide showed various organisms.
The Solution:
- Date of MyPerioPath® (Pre-Therapy) and Celsus One™ Tests: 7/20/2020
- Periodontal Therapy: Two back-to-back appointments consisted of full mouth debridement, full mouth scaling and root planing (SRP), periodontal charting, Triology® serum, and full mouth ozone. Concluded therapy following 6 weeks of healing.
- Systemic Antibiotic Used: Considered but not administered.
- Home Care: To the existing home care added the Viajet oral irrigator, Perioscript™ twice a day in the water irrigator, smart floss daily, copper tongue cleaner, Triology rinse and Olive Gold 03® (ozonated olive oil).
- Date of MyPerioProgress® (Post-Therapy) Test: 9/1/2020
The Result:
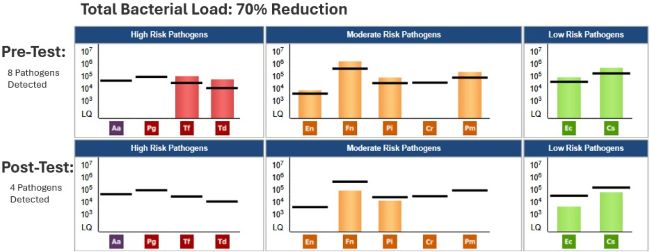
Upon assessment at the follow-up appointment, the pocket depth reduction and bleeding were reduced significantly and the interdental papilla between tooth #8 and #9 showed great improvement. Overall, the patient expressed enormous satisfaction with this resolution. The therapy produced a 9% overall reduction of the pathogens which was measured by MyPerioProgress results. With the minimal reduction of bacteria, but significant resolution of clinical signs, the emphasis is placed on the home care regimen and regular maintenance visit. Celsus One shows a minimal risk of relapse due to her own inflammatory response. The goal is to be able to establish home care habits to assist the patient's remission and reinforce the need for recall, not just for oral health, but overall wellbeing.
About the Author:

Daniela Yanez received her Associate of Science in Dental Hygiene from Palm Beach State College. Originally from Ecuador, she has resided in Florida for the past 20 years. She brings 14 years’ experience to her lead dental hygienist position with Dr John D Light DMD Holistic Practice. She is committed to improving and maintaining the oral and whole-body wellbeing of every patient with a holistic approach. In her free time, she participates in mission trips to deliver care to those most in need.
![Thumbnail [200x250]](img/case-study/Class%20II%20Periodontitis%20and%20Mouth%20Breathing_124787499_v2.jpg)
Class II Periodontitis and Mouth Breathing
The Challenge:
To establish health through periodontal intervention per JP Institute protocols.
The Background:
- Age: 25
- Sex: Female
- Medical History: Adderall controlled ADHD with panic disorder
- Family History: Father: early Cardiovascular Disease; Maternal Grandmother: periodontal disease and high decay rate; Maternal Grandfather: died in his 60's of fatal myocardial infarction, history of transient ischemic attack, oral cancer and lung cancer
- Last Dental Exam: 3/02/2016
- Chief Complaint: Gums hurt and bleed, bad breath, mouth breathing
- Clinical Assessment: Referral to periodontist 3/2/2016. Diagnosed with Localized Aggressive Periodontitis. Recommended Treatment: Surgery with fair prognosis. Patient scheduled for surgery but canceled the appointment. Recommended third molars extracted, but never scheduled.
- Periodontal Assessment: Generalized 4-5mm pockets with bleeding, localized 6-9mm pockets, radiographic bone loss.
The Solution:
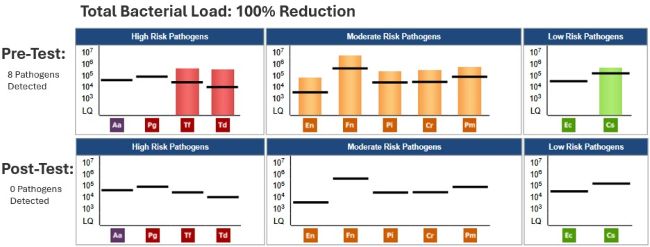
- Date of Pre MyPerioPath® (pre-therapy test): 4/20/2017
- Periodontal Therapy: 6-8 one hour Periodontal Therapy Visits, Micro-ultrasonic technology, Oral Irrigation, Extraction of partially erupted 3rd molars.
- Systemic Antibiotic Use: Metronidazole 500mg bid for 8-10 days
- Home Care Instruction: Sonicare Toothbrush & Sonicare Airflosser, StellaLife® rinse and gel, LifePak® Nano
- Date of MyPerioProgress® (post-therapy test): 8/30/2017
Additional Comments: The post therapy test was ordered as an Alert 2™. Nutritional Counseling was also administered.
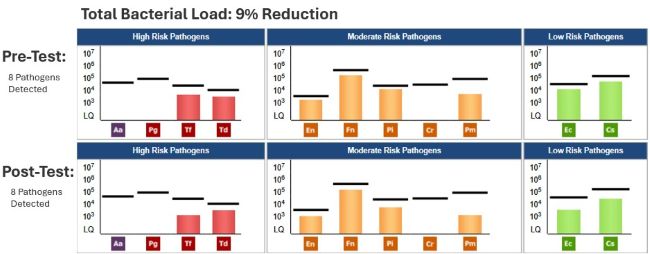
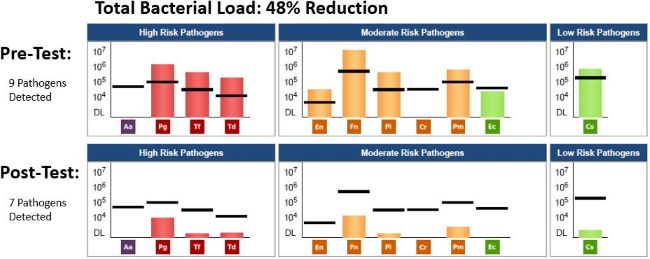
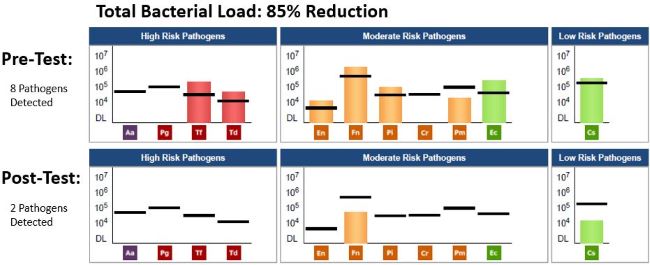
The Result:
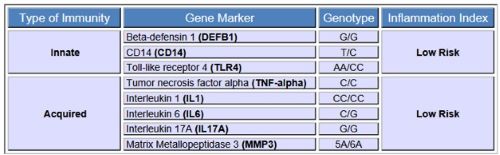
By incorporating OralDNA salivary tests, the pre-test MyPerioPath, and integrating The JP Institute methods of communication, my patient was able to own her disease. The pre MyPerioPath confirms a bacterial cause and the post MyPerioProgress gives an objective measurement of bacteria reduction. The MyPerioID® portion of the Alert 2 being G/G, or High risk, helps to establish the need for more comprehensive non-surgical therapy and frequent re-care as well as forewarns the patient of possible relapse.
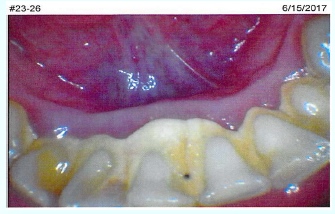
I was confident the periodontal therapy was going to result in a healthy tissue response, which is apparent from the below photo. The patient and I were pleasantly surprised with the overall health benefits including improved energy, better breathing- as her sinuses cleared resulting in secession of mouth breathing, and her mood stabilized resulting in discontinuation of Adderall.

About the Author:

Annie-Laurie Harris BSDH, RDHMP has been in clinical practice for 22 years. Her career began in a progressive periodontal specialty practice where she developed a fascination for the treatment and maintenance of periodontal disease. She was introduced to a philosophy and technique that was innovative and successful in treating periodontal disease. She received intensive training from the JP Institute in Evolutionary Hygiene in 2004. In 2008 she completed JP Institute's Mastership program. She is also currently pursuing a Master's Degree in Dental Hygiene Research at Old Dominion University.
She became a founding member of the American Academy of Oral Systemic Health. This discovery ignited an enthusiasm for the science and treatment of biofilm. Her colleagues and patients have given her the affectionate nick-name 'Dental Geek'. She has been known to attach a head cam to demonstrate (to her willing patients) live video of the biofilm disruption process. Annie is thrilled to be mentoring and training to her fellow colleagues and considers herself a JP Institute Evangelist.
![Thumbnail [200x250]](img/case-study/Class%20II%20Generalized%20Periodontitis%20and%20Rheumatoid%20Arthritis%20Requesting%20Implant%20Placement_328261126-RESIZE.jpeg)
Class II Generalized Periodontitis and Rheumatoid Arthritis Requesting Implant Placement
The Challenge:
To establish periodontal remission by addressing the clinical manifestations of periodontal disease and altering the oral flora in order to lower the incidence of periodontal disease relapse. Bacterial management will eliminate a source of total body inflammation and increase success of implant placement.
The Background:
- Age: 66
- Sex: Male
- Medical History: Rheumatoid arthritis, takes Lisinopril
- Last Dental Exam: 05/16/2019
- Home Care: Brushing twice a day and sporadic flossing
- Chief Complaint: Missing tooth #19 and interested in dental implant
- Clinical Assessment: Class II generalized periodontitis with localized Class III periodontitis. Generalized bleeding on probing and localized bulbous and erythematous tissue on buccal aspect of tooth #5 due to excess material on Class V restoration.
- Periodontal Assessment: Upon probing and completion of periodontal assessment, this case was classified as Class II generalized periodontitis with localized Class III periodontitis due to pocket measurement on mesial of #14.
Additional Comments: Patient indicates he visits the dentist every six months and reports no previous periodontal treatment.
The Solution:
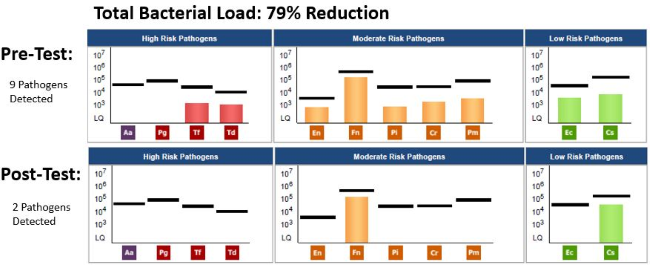
- Date of Pre MyPerioPath® (pre-therapy test): 05/16/2019
- Periodontal Therapy: Patient was scheduled for full mouth debridement and localized curettage on periodontal pocket sites. This procedure was performed for 3 consecutive weeks and pockets were stabilized to measurements 2-3mm.
- Systemic Antibiotic Use: A script of Amoxicillin 500mg, 3 times a day for 7 days was prescribed even though all bacteria were under reference lines.
- Home Care Instruction: Perio Protect™ trays were recommended for use twice a day with Perio Gel® for 15 minutes each application for 3 weeks, then every other day until 3 month follow-up. Oral hygiene instructions on how to brush and floss correctly were reinforced.
- Date of MyPerioProgress® (post-therapy test): 09/03/2019
The Result:
Clinically there was 100% pocket size reduction on pockets greater than 3mm. All periodontal pockets stabilized and zero bleeding on probing was observed. There was a 79% reduction in periodontal pathogen (burden) load 3 months and 18 days after treatment started. These current results are likely associated with a decrease in both oral and systemic inflammation. Having clinical improvement is always our goal and was achieved in this case. The significance of having the pre and post therapy MyPerioPath results gives me an objective measurement to things I can’t visually see. With the reduction of bacterial load, I now know the environment for surgical placement of an implant has less risk for failure due to periodontal pathogens. I utilize this test as a pre-surgical work up, just like a medical doctor uses blood work before their hip/knee/valve replacements surgeries.
About the Author:

Dr. Patricia Lugo is a Puertorriquena oral surgeon who studied her doctorate degree at University of Puerto Rico Medical Sciences Campus and has been practicing for more than 10 years in the private sector. Her passion is practicing Complete Health Dentistry, dentistry that links oral health with systemic health. She works with her husband, Dr. Edwin Rodriguez, prosthodontist, on providing optimal health to patients with complex oral rehabilitations.
![Thumbnail [200x250]](img/case-study/case_williamson/williamson_main.jpeg)
Classic Periodontal Disease Reaches Remission
The Challenge:
Several years of periodontal neglect revealed significant disease.
The Background:
- Age: 48
- Sex: Female
- Medical History: Autoimmune arthritis, chronic sinusitis
- Last Dental Exam: 10/04/2018
- Chief Complaint: Broken lower left molar with swelling. However, a recent course of antibiotics for the sinus infection reduced the swelling temporarily.
- Clinical Assessment: Per the cone-beam computed tomography (CBCT) systems scan, several teeth have periapical abscesses on #2 and 14 and furcation involvement on #18 and #19.
- Periodontal Assessment: Generalized moderate to heavy radiographic subgingival calculus with generalized horizontal bone loss with localized vertical bone loss.
The Solution:
- Date of MyPerioPath® (Pre-Therapy) Test: 10/04/2018
- Periodontal Therapy: Scaling and root planing (SRP) was performed 1/2 mouth each time with 1 week in between. SRP consisted of ultrasonic and iodine flush.
- Systemic Antibiotic Used: The patient started Amoxicillin and Metronidazole per MyPerioPath results after the first 1/2 SRP was completed. Instructed the patient to take a probiotic 2 hours after and 2 hours before the systemic antibiotic dose.
- Home Care: Antiseptic mouth rinse 2x/daily swishing for 30 seconds and not rinsing for 30 minutes after. Use proxybrush daily and electric toothbrush 2x/day.
- Date of MyPerioProgress® (Post-Therapy) Test: 1/15/2019
Additional Comments: Several extractions were completed following the periodontal therapy.
The Result:
At the post-therapy appointment, the tissue appeared pale pink and firm. There was no soft plaque present, the patient was compliant with the home care instructions. The success of this case is directly related to the patient's compliance of completing all proposed treatment in a timely manner. She had failing teeth due to localized severe periodontal disease; by removing the teeth and starting the systemic antibiotics in conjunction with SRP, we were able to stabilize her periodontal health. With comprehensive treatment completed in a chronological order, there was not any time for cross contamination or re-growth of bacteria, therefore eradicating the periodontal infectious bacteria.
About the Author:

Kristi Williamson, graduated from OIT in 2007 and has obtained an expanded functions and laser certification as a Registered Dental Hygienist. She has worked for Dr Mayes since 2013. Kristi is happily married with two kids and was born and raised in the Grande Ronde Valley.
![Thumbnail [200x250]](img/case-study/Class%20III%20Moderate%20Periodontitis%20with%20Halitosis%20Case%20Study%2030%20Percent%20Fade_68322631.jpg)
Class III Moderate Periodontitis with Halitosis
The Challenge:
To reduce periodontal pathogens, a significant cause for the periodontal inflammation and halitosis.
The Background:
- Age: 61
- Sex: M
- Last Dental Exam: 3 months ago
- Home Care: Manual toothbrush daily and flossing on & off
- Chief Complaint: Halitosis
- Periodontal Assessment: Type III generalized with localized Type IV periodontitis. Patient has history of periodontal therapy in past with 3 month re-care intervals. The patient had generalized heavy, bleeding on probing and tissue was bulbous & erythematous.
The Solution:
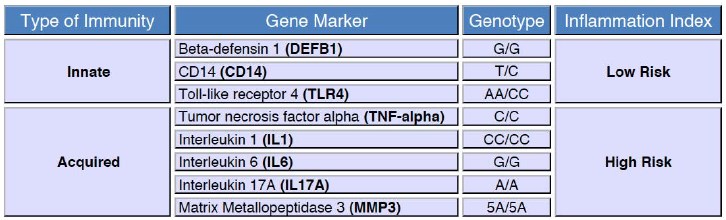
- Date of Pre MyPerioPath®, Celsus One™ and OraRisk® HPV on 7/13/2017
- Periodontal Therapy: Initially recommended 12 hrs of non-surgical periodontal therapy due to Celsus One High Inflammation Index. However, only 4 hrs were needed due to patient’s home care compliance (see Home Care below). The therapy consisted of microsonics, irrigation and laser therapy.
- Systemic Antibiotic Used: It was considered but due to the patient's favorable response to non-surgical, it was never administered.
- Home Care: PerioProtect™ trays 2-3x/day with a vibramycin (doxycycline gel) for 6 weeks initially. Following the non-surgical periodontal therapy, PerioProtect trays 2x/day with 1.7% peroxide gel, Waterpik® daily and electric toothbrush 2x/day.
- Date of MyPerioProgress® (post-therapy test): 11/09/2017
The Result:
Clinically there was a significant decrease in bleeding on probing and pocket depth reduction was amazing. The MyPerioProgress showed pathogen reduction from 8 above reference line to 0. I enjoy seeing the patient’s reaction when they realize they have some control over what is happening. When they do the expected increased home care and reduce therapy time, they are thrilled. This re-enforces home care for maintenance. In this case, the patient’s partner was tested and revealed periodontal pathogens very similar to this patient, however the partner has refused treatment at this time. This places our patient at risk for relapse especially due to the Celsus One results.

About the Author:

![Thumbnail [200x250]](img/case-study/LIGHT%20Class%20II%20Periodontitis_130547494.jpg)
Class II Periodontitis
The Challenge:
The patient has Class II periodontitis with a lack of home care and recall. Through periodontal therapy, our goal is to establish a remission of the disease and establish a healthier bacterial load to reduce oral/systemic complications. Through education, our goal is to establish home care habits to assist patient’s remission and stress the need for recall not just for health of periodontium but overall health.
The Background:
- Age: 54
- Sex: F
- Medical History: High blood pressure and allergy to penicillin
- Family Medical History: Diabetes, cardiovascular disease, stroke and cancer
- Last Dental Visit: 6 years ago
- Home Care: Manual toothbrush 1-2x per day with occasional antibacterial mouth rinse and tongue brushing
- Nutrition: Diet soda daily, tea with honey
- Patient Chief Complaint: “Bleeding gums when brushing, possible cavities and tooth crowding.”
- Clinical Assessment: Deteriorating margins of amalgam restoration, recurrent decay diagnosed by exam and radiographs. Generalized plaque with moderate calculus.
- Periodontal Assessment: Class II periodontitis. 110 out of 168 points of bleeding, all 28 teeth with generalize 4 mm probe depths with localized 5mm probe depths. Bone loss of 1-10% including both horizontal and vertical throughout.
The Solution:
- Date of Pre MyPerioPath® (pre-therapy test): 6/15/2017
- Periodontal Therapy: 4 quadrants scaling and root planning and doxcycline subgingivally in all areas.
- Systemic Antibiotics Used: Ciprofloxacin & Metronidazole per results
- Home Care: Chlorhexidine rinse at home 2x daily
- Date of MyPerioProgress® (post-therapy test): 10/5/2017
The Result:
At the 6-week tissue check, this patient has been using an electric toothbrush 1-2x per day, flossing a couple times per week, utilizing a tongue scraper, and using the chlorhexidine mouth rinse. Patient discontinued the rinse after 2 weeks due to increasing sensitivity. Post-therapy periodontal charting was completed with 1 localized 4mm residual pocketing and 12 out of 168 bleeding on probing. The post therapy MyPerioPath saliva sample was collected. A prophy, polishing, flossing was also completed. Patient will be seen every 3 months for periodontal maintenance. MyPerioProgress results showed reduced periodontal pathogens reductions from 7 pathogens above reference lines to 0 above. The patient was called, and results were reviewed, she then received a copy to give to her medical doctor.
About the Author:
