Challenge: Our case study represents an example of the emerging evidence from interventional and, more recently, animal studies showing how seemingly unrelated diseases such as periodontal disease and rheumatoid arthritis can be related through similar genetic, biological, and clinically consistent mechanisms.1,2,3,4
Background: The initial medical assessment for a 57-year-old female diagnosed with palindromic rheumatoid arthritis was conducted at our functional medicine clinic. Before beginning our guided therapy, the patient expressed the desire to explore self-guided alternative treatment. After 6 months, the patient returned unhappy with her attempt at alternative treatment.
During the medical re-assessment following the 6 months, there was no change in pain and soreness around the joints. CRP increased from 19.4 to 26.2 with an increased ESR to 46. In addition, a large Baker’s cyst developed on the right knee accompanied by a swollen right ankle with reduced feeling to the right foot. Stiffness also spread to the right wrist and several finger joints in both hands.
Medical Perspective: If you follow the research, you must ask about the patient’s dental health. We are not trained to be experts on oral health. However, we have the capability to run laboratory tests such as MyPerioPath®, dnasmile, and activated MMP8 to gain additional insight. “It must be standard of care in every functional medicine practice to at least ask the question about your patient’s dental health” is something we practice, and thankfully we have a working relationship with Dr. Victoria Sampson BDS MFDS RCS Ed, a Functional Dentist in London. This patient was referred for oral evaluation following MyPerioPath® testing in office.
Oral Background: Upon assessment, generalized plaque, severe levels of bleeding on probing, generalized 40% radiographic bone loss, probe depths ranging from 2mm-7mm and furcation involvement was discovered periodontally. Additional testing was performed revealing elevated activated MMP8 and lots of vitamin B issues.
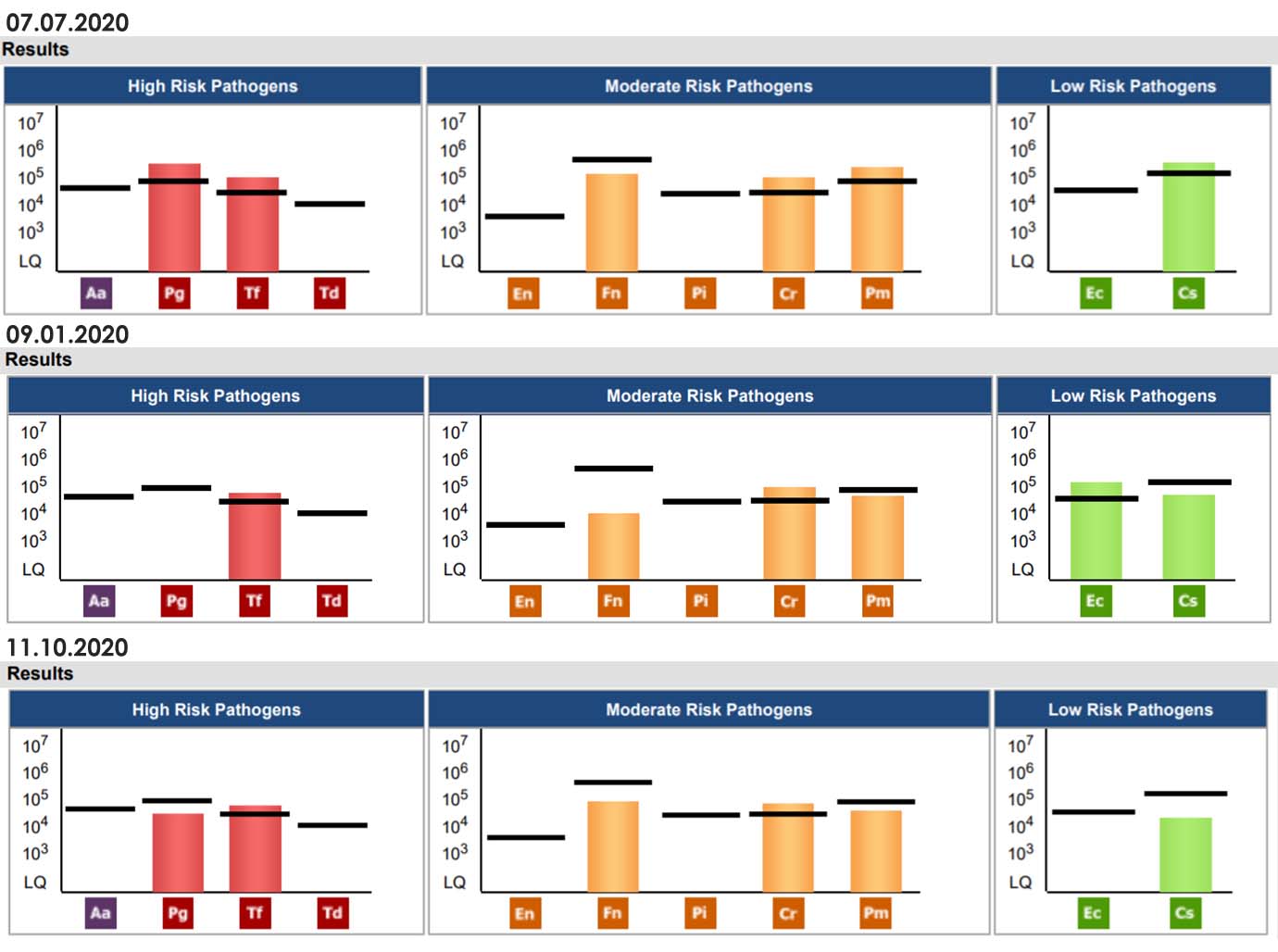
Solution: In addition to the plethora of active disease clinical signs, the elevated activated MMP8 43.16, and MyPerioPath® results (below), led to a treatment plan of guided biofilm therapy every 2-3 months. Home care instruction included use of a remineralizing toothpaste and antiseptic mouthwash, TePe™ brushes (interdental), floss twice a day and brush twice a day with an electric toothbrush. A tongue scraper in evening was introduced. Medically, dnasmile results helped give a more personalized dietary approach with an anti-inflammatory focus including curcumin, Omega 3 oil, increase phytochemical density and with variety of real whole food, green tea and collagen. Follow up testing with MyPerioPath® was conducted at 2 months and 5 months of applied therapy.
Results: At 8 weeks post dental and functional medicine treatment, patient observed a decrease in swelling and joint soreness, especially in her hands and wrists. Her perception of daily pain significantly reduced. The Baker’s cyst reduced in size approximately 50%. CRP dramatically improved, reducing from 26.2 to 4.8. With the increased bacterial load (see MyPerioPath® below) but reduced disease activity (MMP8 40-MMP8 <10), we theorize that, based on the oral genomic data, more bacterial interventions will continue to calm local and systemic inflammation and modulate acquired immunity, continuing to reduce active periodontal disease and systemic inflammation.
The right practitioner plus the right dentist plus the right tests (oral & genetic diagnostics) will reduce the disease process.
References:
- Potempa, J., Mydel, P. & Koziel, J. The case for periodontitis in the pathogenesis of rheumatoid arthritis. Nat. Rev. Rheumatol. 13, 606–620 (2017).
- Fuggle NR, Smith TO, Kaul A and Sofat N (2016) Hand to Mouth: A Systematic Review and Meta-Analysis of the Association between Rheumatoid Arthritis and Periodontitis. Front. Immunol. 7:80. doi: 10.3389/fimmu.2016.00080
- Arthritis – Basics – Definition – Rheumatoid Arthritis (2015). Available from http://www.cdc.gov/arthritis/basics/rheumatoid.htm
- McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med (2011) 365(23):2205–19. doi:10.1056/NEJMra1004965
To inquire about DNA Smile email: pete@fm.associates
For more information on how to become an OralDNA Provider – scan HERE: 
- Interview with Functional Medicine, International Leader Pete Williams - November 25, 2022
- Periodontal Disease and Rheumatoid Arthritis – Controlling Two Birds with One Stone? - September 10, 2021
- Interview with Functional Medicine Leader, Pete Williams - July 12, 2019