Challenge: To reduce periodontal pathogens in the oral cavity that are contributing to severe periodontal inflammation and tissue sensitivity.
Background: The patient is a 33-year-old female with a history of treatment for ovarian cancer. The patient presented with severely inflamed gingiva with generalized extreme heavy bleeding upon gentle probing. Upon touch, there was generalized sensitivity. For the patient’s home care routine, she states that she practices daily toothbrushing and infrequent flossing. Using information found during the periodontal assessment, the patient was classified as Class I generalized periodontitis at Stage B. The probe depths were moderately involved, all four millimeters or below, but the extreme bleeding was of concern. The patient has no periodontal treatment in her history but does admit to infrequent visits to any dentist.
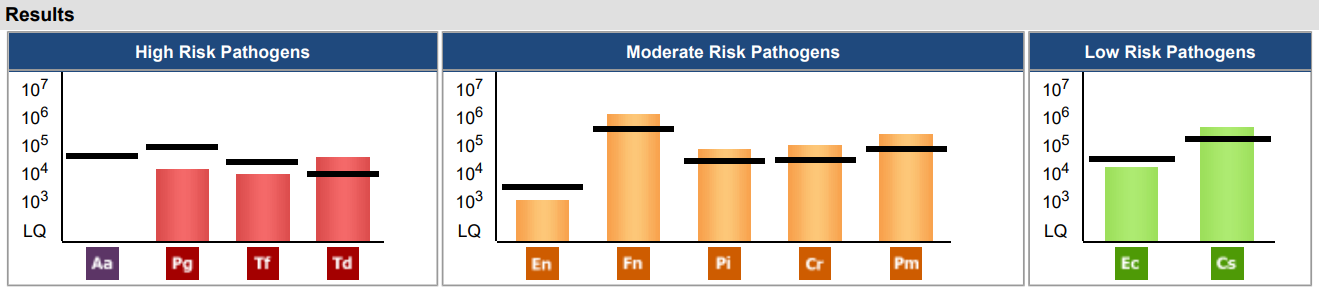
Solution: The sample collection for the OralDNA® MyPerioPath® test was used to confirm the diagnosis and to identify bacterial pathogens that could be contributing to the extreme inflammation and bleeding. Almost all pathogens that were tested for were present in the patient’s oral environment. The results showed one high risk pathogen, Treponema denticola (Td), and four moderate risk pathogens (Fusobacterium nucleatum (Fn), Prevotella intermedia (Pi), Campylobacter rectus (Cr), Peptostreptococcus (Micromonas) micros (Pm)) above the reference lines. These pathogens are associated with chronic periodontitis. These high risk and moderate risk pathogens are risk factors for potential systemic diseases, such as atherosclerosis, type 2 diabetes, arthritis, and various forms of cancer. Because this patient has had a history of cancer and cancer treatment, immunosuppression issues are a likely factor in the build-up of such different pathogenic bacteria. Typically, there would be bone loss associated with these levels and her complicated medical history. The good news is bone loss has not occurred with this patient.
Performing a full periodontal debridement to achieve reduced pathogens and promoting a healthy oral environment was essential to helping this patient reduce inflammation and sensitivity. The patient’s treatment was completed in four appointments. The non-surgical periodontal treatment consisted of full mouth debridement with an ultrasonic, hand instrumentation, and laser-assisted bacterial reduction therapy. To help ensure the management of a healthy oral environment, the patient’s home care routine was modified to include proper toothbrushing techniques twice a day and flossing once day.
Results: A significant decrease in bleeding upon probing was noted already at the first few appointments during treatment. After the patient had received all treatments needed to finish her periodontal therapy, it was riveting to see such drastic improvement. Bleeding upon probing was greatly reduced! The previously inflamed and irritated gingiva was flat and healthy. The patient stated that she has been making sure to brush properly twice daily and floss more frequently. Although it is impossible to remove all bacteria from the mouth, the goal is to find a balance point where the pathogens aren’t causing harm. From the decrease, and in some areas the absence of any clinical signs, we are heading in the right direction to a much healthier overall oral environment.
In summary, it would be beneficial to perform a post-treatment MyPerioPath® analysis along with consistent periodontal maintenance visits for this patient. Overall, this experience with OralDNA® Labs salivary testing was very eye-opening and a fantastic learning opportunity. I hope to be able to use this amazing resource throughout my dental hygiene career. It is a great way to understand and confirm potential causes of oral disease and help to create the best treatment plans for patients.
Would you like to view more case studies? Click here and choose a category.