Challenge: To reduce periodontal pathogens in the oral cavity that are contributing to severe periodontal inflammation, improve oral malodor as reported by the patient and remove unsightly calculus buildup that is harboring oral pathogens.
Introduction: In Fall of 2021, I had the pleasure of learning about OralDNA® Labs’ testing from my instructor Jamie Griggs of Colorado Northwestern Community College (CNCC). Before knowing anything about OralDNA® or how the process works, I wondered why someone would want to test with OralDNA®? After understanding how OralDNA® testing works, I became instantly interested to learn more, not only for myself as a future hygienist, but to learn how I could help my potential patients. Before starting dental hygiene school, I have always heard that there is a connection between oral health and overall health, but I never really understood how or why. Now, after having the opportunity to learn more about OralDNA® tests and being able to use a testing kit on one of my personal patients, I am excited to share my patients’ case.
Background:
- Female patient, age: 24
- Medical History: Patient is overall healthy, last Blood Pressure was 128/78. Patient has been diagnosed with bipolar and Autism. Patient is currently taking Haloperidol for Bipolar and uses an albuterol in inhaler as needed (PRN). Patient also reports use of recreational marijuana daily.
- Family History: Patient informed me that her family has a history of heart disease.
- Last Dental Exam: Before visiting CNCC dental hygiene clinic, the patient’s last dental exam was in 2021 to extract #31, but before that the patient’s last adult assessment and diagnosis was in 2014.
- Home Care: Before visiting CNCC dental hygiene clinic, the patient has minimal daily oral habits that consisted of brushing 1x/day and never flossing.
- Chief Complaint: #17 bothers the patient daily because food gets impacted, and it gives off a bad odor. The patient also does not like the way her mandibular anterior teeth look, due to discolored calculus build up around the margins of the teeth.
Clinical Assessment:
- Gingiva Color: Generalized erythematous, edematous and localized cyanotic both lingual and facial sextant 5
- Margin: Generalized rolled and localized bulbous facial sextant 5
- Papilla: Generalized blunted
- Consistency: Generalized soft
- Texture: Generalized smooth
- Perio reading: Generalized at CEJ and localized recession facial sextant 5
Periodontal Assessment: Stage I Grade B based off assessment, perio readings and radiographs
Solution:
- MyPerioPath test pre therapy: 10/21/21
- Dental therapy: Full mouth non-surgical periodontal therapy (NSPT)
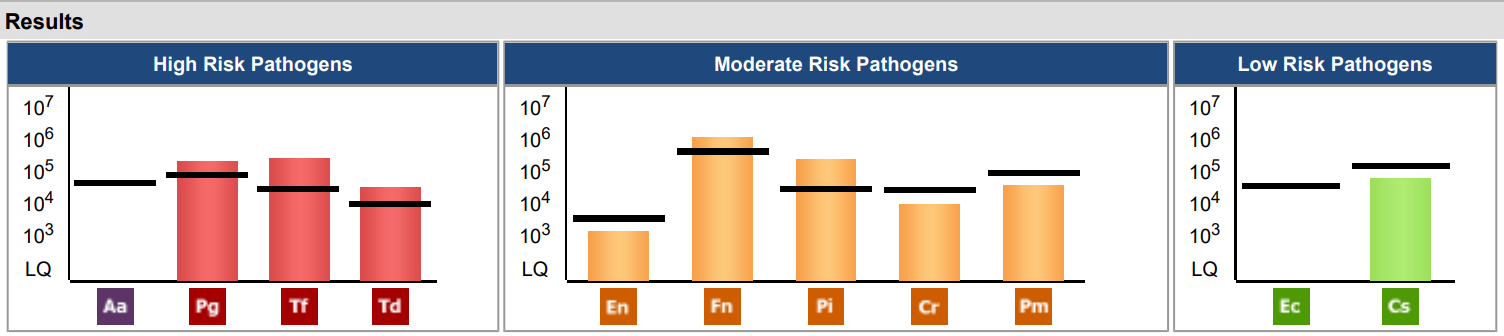
Results: My patient and I were able to sit down together and have a conversation about her MyPerioPath® results and she was able to understand and see the different high, moderate, and low risk pathogens that were present in her oral cavity. I noticed a shift in my patient’s mindset about her oral health, especially after I was able to show her the lab results and connect the different pathogens that relate to other possible systemic diseases such as cardiovascular disease. After my patient saw and learned this information, it was a big connection for her personally because she noticed that the pathogens in her mouth could possibly also be related to her family’s history of cardiovascular disease. I am grateful for the opportunity that I was able to present my patient with her OralDNA® results and I am now confident that I can use OralDNA® testing in my tool kit as a future hygienist to help my patients understand the connection between their oral health and overall health.
Would you like to view more case studies? Click here and choose a category.