 Patient Bio: Your 54-year-old female patient of record has been absent from your practice for 5 years. At the last appointment in 2018, this patient was going through a divorce, and it was recommended that the patient receive periodontal therapy. Now, the patient is emotionally and physically ready to address any concerns as she is caretaker for her mother who has Alzheimer’s. She is taking medication for blood pressure and fluctuating hormones. She does express an occasional bout of brain fog.
Patient Bio: Your 54-year-old female patient of record has been absent from your practice for 5 years. At the last appointment in 2018, this patient was going through a divorce, and it was recommended that the patient receive periodontal therapy. Now, the patient is emotionally and physically ready to address any concerns as she is caretaker for her mother who has Alzheimer’s. She is taking medication for blood pressure and fluctuating hormones. She does express an occasional bout of brain fog.
How would you introduce therapy including MyPerioPath® to this patient?
Mrs. Doe, welcome back to the practice! Last time you were in, we identified that you have periodontal disease and after today’s assessments, we have confirmed that the disease has not resolved. This is typical of gum disease, as homecare alone is generally not enough to treat it. Now that you are ready to move forward with treatment, I highly recommend we start with a simple, 30-second salivary test that is going to help identify which pathogens (bacteria and yeast) are contributing to your condition. We have found this information to be valuable in not only directing treatment, but in helping identify and manage the risk for other systemic diseases such as cardiovascular disease and Alzheimer’s. Given your personal and family history, this could be valuable information that could change the trajectory of your health as you age.
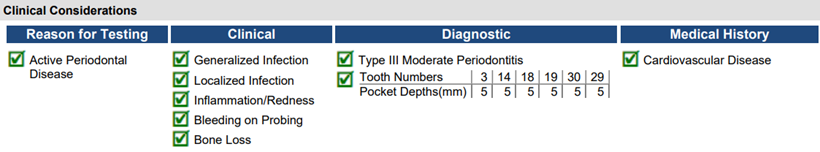
How would you discuss these results with your patient?
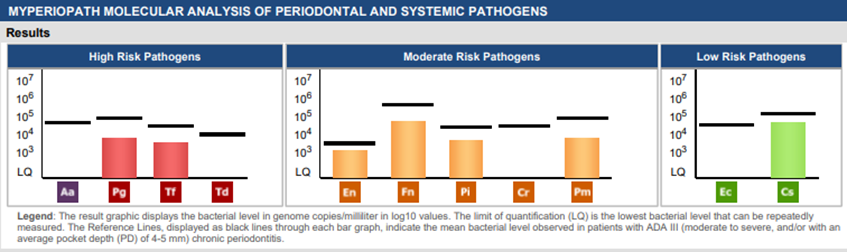
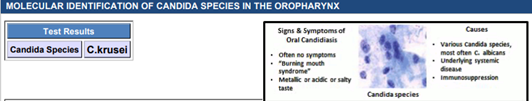
Mrs. Doe, I’m so glad we performed the OralDNA® test prior to treating your periodontal condition. Your test results indicate that there is an unhealthy balance of bacteria and yeast in your mouth. I like to compare this to a garden; every garden has weeds, but problems arise when the weeds outnumber the plants in the garden. Our job is to help rebalance the environment of the mouth so that the good, healthy microbes can flourish. In order to do this, we have to treat the yeast and bacteria simultaneously because they have a symbiotic relationship and work together.
Yeast is one of those “weeds” that exists in our normal flora but can overgrow given the right environment. Often, yeast will overgrow when the mouth becomes too acidic, there’s too much sugar in the diet, and/or when the immune system is challenged.
When looking at your MyPerioPath® results, you’ll see these colored bars. Anywhere there is a colored bar indicates the presence of a bacterial pathogen. The taller the bar is, the greater the risk of periodontal disease activity and certain systemic illnesses. This means that by effectively reducing the height of these bars and/or eradicating them, you will have better control of your oral and systemic health. For you, this is especially important because your results indicate the presence of pathogens that contribute to cardiovascular disease and Alzheimer’s/cognitive decline.
Additional insights:
Our goal is to not only get you through this acute phase of treatment, but to help you achieve long-term, sustainable results. Given the multi-factorial nature of periodontal disease, this means creating a treatment plan that goes beyond the scope of just the mouth. Recommended treatment would include the following:
- Disinfecting and rebalancing the oral microbiome
– NSPT, full mouth laser disinfection, antibiotics, probiotics with S.boulardii (to help manage yeast and prevent antibiotic-induced GI upset), CTx4 Rinse, thorough homecare (Electric toothbrush and Waterpik® w/ 6-8 drops of bleach) - Managing the host-immune response (how your body responds to microbial challenge)
This requires further investigation into the following:
– Quality of sleep
– Breathing (Nasal/Mouth? Fast/Slow? Shallow/Deep?)
– Diet (Sugar Consumption? Nutritional Deficits? Referral to Functional Nutritionist?)
– Genetics
**This treatment plan is always tailored to the patient’s readiness and goals for treatment. All recommendations can be modified to fit each individual person**
- How Do You Speak Testing? With Emily McCleary, RDH - June 16, 2023