How the heck are we supposed to implement the new American Academy of Periodontology (AAP) Staging and Grading Periodontitis classifications into practice? This new system seems so complicated, right?? Actually, it can be simplified and once that is done, the new system is extremely valuable! As hygienists, we know that periodontal disease is multifactorial. It is affected by systemic health, habits, occlusion, and more. We know that it is just as much about the host response as it is about bacteria. The new classifications help us categorize these factors in a comprehensive way. Once you understand it, you will love it!
The previous classifications were last updated in 1999. These only looked at the severity of past destruction. The new classifications were updated by AAP and the European Federation of Periodontology (EFP) at the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Disease and Conditions. The new guidelines look at severity of past destruction as well as missing teeth, complexity of managing the case, future risk of progression, likelihood of responding to standard therapy, and potential influence of periodontitis on systemic health.
The new system can seem daunting, but there is a manageable way to approach it that makes it much easier. First, the classifications are divided into 3 buckets. 1. Health and Gingival disease, 2. Periodontitis, and 3. Implant health and disease conditions. A big difference to note here, is that Gingivitis is no longer Stage 1. It is simply gingivitis caused by biofilm, or gingivitis not caused by biofilm. Implants are considered separate from natural teeth. Their classifications are peri-implant health, peri-implant mucositis, peri-implantitis and peri-implant hard and soft tissue deficiencies. The hard and soft tissue deficiencies are considered to be due to improper placement of the implant.
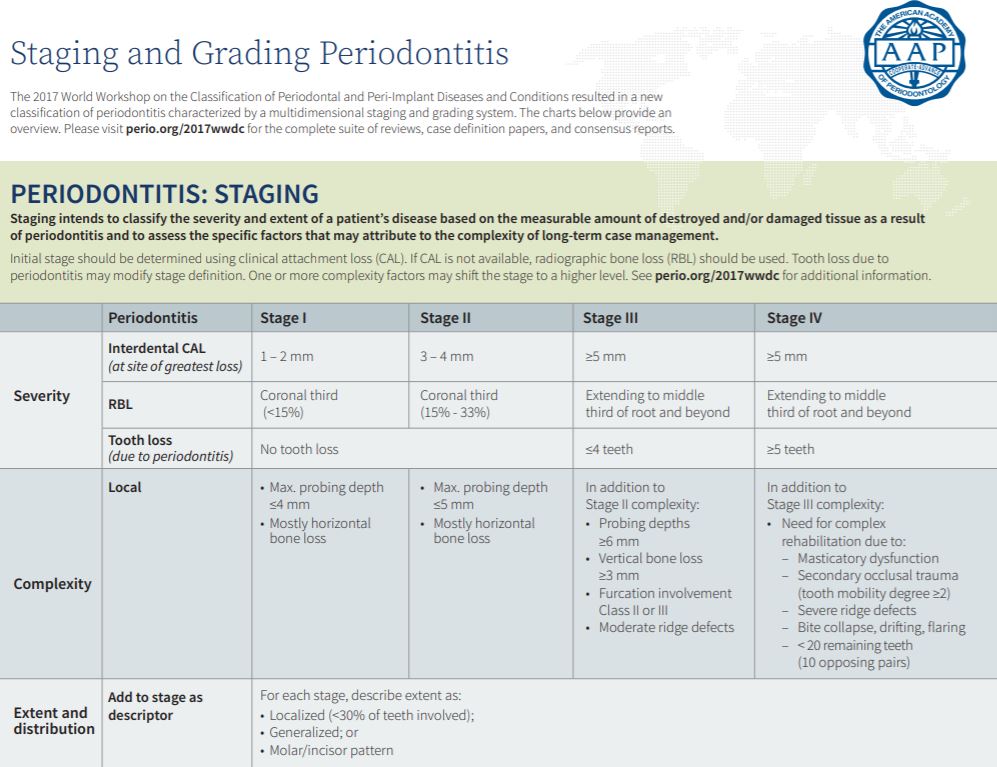
In order to classify periodontitis, follow these three steps. Establish a stage, determine a grade, and decide on a distribution. When determining the stage and grade, always base your diagnosis on the worst site in the patient’s mouth.
Let’s start with Staging. The Stages are divided into 4 categories: Stage 1-Mild, Stage 2-Moderate, Stage 3-Severe with the potential for tooth loss, and Stage 4-Severe with the potential for dentition loss. The AAP recommends starting by choosing either between Stages 1 and 2, or between Stages 3 and 4. Ask yourself, has this patient lost any teeth, or do they have the potential to lose any teeth due to periodontitis? If the answer is no, then you will place them in either Stage 1 or 2. If yes, then they will be in either 3 or 4.
Stage 1 presents with pocketing <4mm and 1-2mm of clinical attachment loss (CAL) and radiographic bone loss <15%. Stage 2 presents with pocketing <5mm and 3-4mm of CAL with radiographic bone loss from 15-33% and potentially redness, swelling, bleeding on probing, and mostly horizontal bone loss with no mobility, furcations, or missing teeth.
Stage 3 and Stage 4 depend on missing teeth. Stage 3 presents with up to 4 missing teeth. Stage 4 presents with 5 or more missing teeth resulting in masticatory dysfunction. There will likely be secondary occlusal trauma, severe ridge defects, mobility of 2 or more, bite collapse, drifting, flaring and less than 20 teeth or 10 opposing pairs. Both stages present with radiographic bone loss >33%, redness, swelling, BOP, possible mobility, furcation involvement, and vertical bone loss.
Staging is only one aspect of the new AAP guidelines. Stay tuned to next week’s blog where we discuss grading and distribution making the AAP Classification simplified.
Reference: The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions was co-presented by the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP). Tables from Tonetti, Greenwell, Kornman. J Periodontol 2018;89 (Suppl 1): S159-S172
For more information on how to become an OralDNA Provider – scan HERE: 
- AAP Classifications Simplified: Part 2 - April 3, 2020
- AAP Classifications Simplified: Part 1 - March 27, 2020

