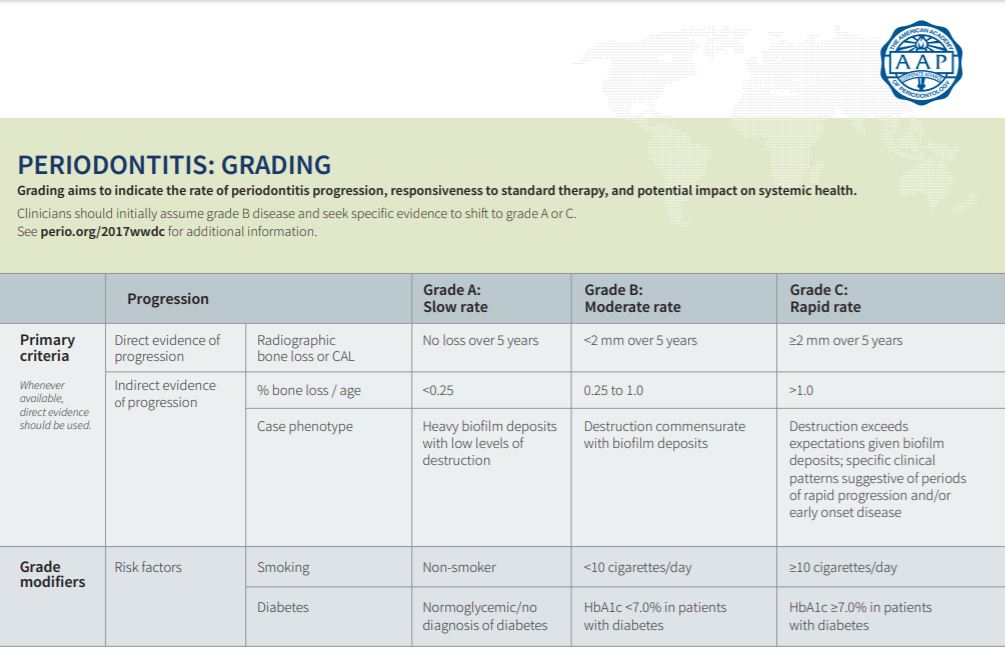
Last week, establishing a stage for your patient was highlighted. Click HERE to review. Once you have established the stage of your patient, the grade needs to be determined. The three grades are A, B or C. The grade indicates the speed of progression and the quality of treatment response. In order to establish the grade, there are 3 factors to consider:
- Direct evidence – Evidence of bone loss over the past 5 years. (You may not have access to previous records, but this highlights the value of forwarding records)
- Indirect evidence – Bone loss compared to the patient’s age and destruction compared to biofilm deposits
- Grade modifiers – Tobacco use and Diabetes
At this point the AAP only considers tobacco use and diabetes as grade modifiers. As hygienists, we know there are more conditions and habits that can complicate periodontal treatment. I consider any auto immune systemic conditions, genetic susceptibility such as detected in Alert 2™ (MyPerioID® IL-6) and Celsus One™ and habits such as vaping or marijuana use as grade modifiers as well. It is important to note that grade modifiers only increase the grade.
The AAP recommends starting with Grade B and looking for a reason to change. Grade B will be the most common and denotes a moderate rate of progression. A patient in Grade B will have direct evidence of progression with less than 2mm of radiographic bone loss (RBL) over 5 years. Indirect evidence of progression would include .25 to 1.0% of bone loss/age and destruction commensurate with biofilm deposits. MyPerioPath® can provide valuable insight when it comes to determining biofilm destruction nature through the measurement of 11 harmful pathogens. Remember, always base your staging and grading on the worst site in the patient’s mouth.
Now, for the grade modifiers. If you determine that a 40-year-old patient has less than 10% bone loss, you will choose Grade A; however, if they are a smoker or a diabetic, then they would be bumped up to Grade B. The same happens if the patient has between 10 and 41% bone loss. If they are a smoker or diabetic, they would be bumped up to Grade C. The grade modifiers DO NOT affect the Stage, they only affect the Grade.
Now, as far as determining the bone loss, the interproximal crests of bone always follow a line along the cemento-enamel junction (CEJ) of each tooth. Healthy bone should have a solidly visible Lamina Dura, and the interproximal crests should be rounded or pointed coronally. If the Lamina Dura is broken or fuzzy, this is early bone loss. If the interproximal crests are pitted or cratered, this is also early bone loss. More severe bone loss is easier to confirm. Divide the root into 3rds starting at the CEJ. If the bone level is in the first 3rd, it is less than 30%, if it is in the second 3rd, it is between 30 and 60% and if it is the last 3rd it is over 60%. Estimate more precisely depending on where in the box the bone loss falls.
Distribution is the final step in classifying your periodontal patient. There will be either generalized, which is greater than 30% of the dentition, localized, which is less than 30%, and molar-incisor distribution. The molar-incisor distribution is rarely used and is typically only seen in rapidly aggressive or juvenile periodontitis.
Here are some examples:
- 40-year-old male presents with no medical issues or medications, no tobacco use or other habits, moderate biofilm deposits, generalized 4mm pockets with bleeding, and visible deterioration of lamina dura and interproximal crests of bone. In the worst site there is roughly 8% bone loss. This patient would be classified Generalized Stage I Grade A periodontitis. This patient would be a candidate for full mouth SRP.
- 51-year-old male presents with uncontrolled diabetes. No tobacco use or other habits, light biofilm deposits, generalized 4mm and localized 5mm pockets. Generalized bleeding and horizontal bone loss with approximately 20% bone loss in the worst site in the patient’s mouth. This patient would be Stage 2 Grade B if there were no grade modifiers; however, due to the uncontrolled diabetes he is Grade C. The distribution is still generalized, because there is generalized bone loss, 4mm pockets, and bleeding. The final classification is Generalized Stage II Grade C periodontitis.
It is also important to consider history of orthodontia and occlusal trauma affecting bone loss. If you have a patient that had ortho, has flat interproximal crests and fuzzy lamina dura, the RBL is likely from the movement of the teeth reshaping the bone. In these cases, treatment plan more conservatively. Also, occlusal trauma can cause bone loss and recession. Consider these factors when determining the stage and the grade.
Here’s the simple breakdown. When classifying a patient with periodontitis, start by determining the Stage between 1, 2, 3, or 4. Once the stage is determined, choose a grade A, B, or C. Start with grade B, then look for a reason to change it, this will simplify the process. Be sure to check medical history for any grade modifiers that could increase the grade. Finally choose a distribution and add it as a descriptor. The standardization of these AAP guidelines along with other supporting documents, such as an OralDNA® Labs’ Alert 2™ report will help communication within our profession and with our patients.
Reference: The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions was co-presented by the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP). Tables from Tonetti, Greenwell, Kornman. J Periodontol 2018;89 (Suppl 1): S159-S172
For more information on how to become an OralDNA Provider – scan HERE: 
- AAP Classifications Simplified: Part 2 - April 3, 2020
- AAP Classifications Simplified: Part 1 - March 27, 2020

