Heart Disease Begins in the Mouth
High sensitivity C-reactive protein (hs-CRP) is the most clear, quantifiable, and readily accessible marker of the oral-systemic connection. We present a case study of an otherwise healthy 62-year-old woman with elevated hs-CRP who had abundant numbers of pathogenic oral bacteria. A natural dental health treatment over two years lowered hs-CRP and lowered oral pathogens. Given the links between oral disease, inflammation, and heart disease, it is wise to test for oral dysbiosis in patients presenting with an elevated hs-CRP.
Case Study
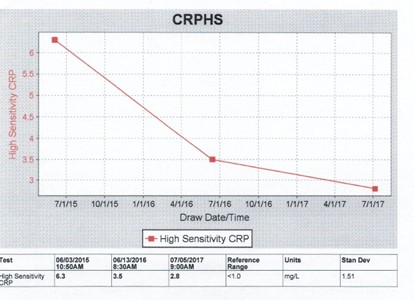
A 62-year-old woman, named “Linda” for the purposes of this case, presented to her family physician for her annual check-up. The integrative medical doctor did the usual battery of tests on Linda, including blood sugar, cholesterol, and hs-CRP. Linda said she was feeling fine and didn’t report any major issues with her health, nor signs of gum disease. Linda’s lab tests came back, and she had high levels of serum hs-CRP, at 6.3 mg/L (reference range <1.0).
hs-CRP is an acute phase reactant produced by the liver. It elevates due to infection, inflammation, or trauma. hs-CRP has been established as an independent predictor for coronary artery disease1 and a key biomarker of systemic inflammation.2 hs-CRP correlates with periodontal disease severity, and decreases after nonsurgical periodontal therapy.3 Finally, an association between periodontitis and cardiovascular disease has been reported in population studies.3
Based on Linda’s high hs-CRP, the practitioner tested Linda’s oral bacteria with the MyPerioPath® test from OralDNA® Labs. She wanted to see if Linda’s elevated biomarker of heart disease might have its origin in the mouth. MyPerioPath® methodology uses real-time polymerase chain reaction (RT-PCR or qPCR) to identify and quantify microbial DNA in an oral rinse specimen.
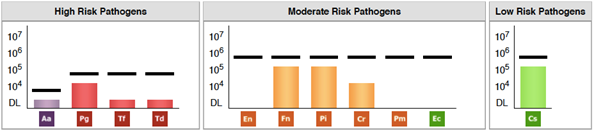
Figure 1. Linda’s first OralDNA®Labs MyPerioPath® report from June 2015, showing numerous oral pathogens, albeit at low levels.
Linda’s MyPerioPath® test showed the presence of eight different periodontal pathogens. Her oral microbiome showed low levels of four high-risk periodontal disease pathogens, three intermediate-risk periodontal disease pathogens, and low amounts of one low-risk periodontal disease pathogen. The oral pathogens detected were: Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tannerella forsythia, Treponema denticola, Fusobacterium nucleatum/periodonticum, Prevotella intermedia, Campylobacter rectus, and Capnocytophaga species.
Linda was immediately started on a protocol to improve her oral health. Linda was already flossing daily and brushing her teeth twice daily. In addition, the practitioner instructed Linda to use a stainless-steel tongue scraper before brushing her teeth. She added GUM® soft picks, once per day, to her flossing regimen. Linda was also directed to add two drops of frankincense essential oil to her Waterpik™ and irrigate her gums once daily.
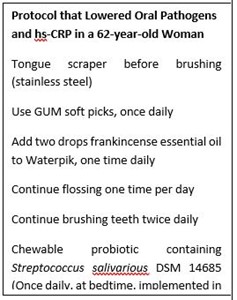
When Linda came back for her annual exam the following year, her hs-CRP had dropped by half. However, it was still elevated. Since her hs-CRP still hinted that there was unchecked inflammation, the clinician advised Linda to continue her protocol with the tongue scraper, the GUM® soft picks, and the frankincense essential oil in the Waterpik. But this time she told Linda to start taking ProbioMax® DDS (Xymogen, Orlando, FL) once per day, at bedtime. ProbioMax® DDS is a chewable probiotic that contains the beneficial oral bacterium Streptococcus salivarius DSM 14685.
Table 1. Levels of hs-CRP in the patient, “Linda,” over the course of treatment. hs-CRP levels dropped into the moderate risk range. A hs-CRP level < 1, 1-3, and >3 is low risk, moderate risk, and high risk, respectively, for global cardiovascular disease.1
| Date | hs-CRP (mg/L) | Reference Ranges (mg/L) | ||
| Low Risk | Moderate Risk | High Risk | ||
| 6/3/2015 | 6.3 | <1.0 | 1-3 | >6.0 |
| 6/13/2016 | 3.5 | <1.0 | 1-3 | >6.0 |
| 7/5/2017 | 2.8 | <1.0 | 1-3 | >6.0 |
When Linda’s physician ordered her routine diagnostic testing the following year (after approximately two years of treatment), everything looked much better. Her hs-CRP was much improved and within the desired range (1-3), yet still not optimal (<1.0 mg/L). Likewise, her oral microbial profile showed improvement, with pathogenic bacteria decreased by half. A. actinomycetemcomitans, P. gingivalis, T. forsythia, and C. rectus were no longer detected at levels deemed to be clinically significant to represent the quantity on the bar graph. Where there were eight different bacteria present in her first test, her follow-up test showed only four. T. denticola and F. nucleatum were still positive. P. intermedia and Capnocytophaga species were still present but were reduced, compared to the first test. Linda’s hs-CRP was much better after treating her oral health and this corresponded with an improvement in her oral microbiome. This suggests that Linda’s systemic inflammation and risk of heart disease was reduced by lowering oral pathogen dysbiosis.
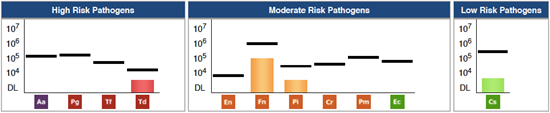
Figure 2. Patient’s follow-up OralDNA®Labs MyPerioPath® report from July 2017, showing dramatic reduction in oral pathogens after two years of treatment.
Conclusions
In this case, a 62-year-old woman without any other major health issues showed high cardiovascular disease risk due to an elevated hs-CRP. Even though she didn’t have any signs of gum disease, oral microbial DNA testing by RT-PCR showed low levels of eight oral pathogens. Integrative medical treatment over two years decreased serum hs-CRP from 6.3 to 2.8 mg/L and decreased the number of oral pathogens to four. By addressing oral dysbiosis and systemic inflammation, as measured by decreasing hs-CRP, this patient may have avoided full blown heart disease. Based on this case and the current evidence, it is recommended to measure and normalize oral bacterial pathogens in patients with elevated hs-CRP as a comprehensive approach to oral-systemic disease. With tongue scraping, soft pics, water flossing with Frankincense essential oil, and S. salivarious chewable probiotics, the clinician treated the oral microbiome, reduced inflammation, and thereby reduced the patient’s risk for stroke and heart attack.
Resources
Physician-Dentist Collaboration Form for patients with elevated hs-CRP, created by Mark Burhenne, DDS.
References
- Kamath DY, Xavier D, Sigamani A, Pais P. High sensitivity C-reactive protein (hsCRP) & cardiovascular disease: An Indian perspective. Indian J Med Res. 2015;142(3):261-268.
- Bansal T, Pandey A, D D, Asthana AK. C-Reactive Protein (CRP) and its Association with Periodontal Disease: A Brief Review. Journal of clinical and diagnostic research : JCDR. 2014;8(7):ZE21-24.
- Mysak J, Podzimek S, Vasakova J, Mazanek J, Vinsu A, Duskova J. C-reactive protein in patients with aggressive periodontitis. J Dent Sci. 2017;12(4):368-374.
We hope you enjoyed the throwback blog. This interview originally posted 11/08/2019.
- Systemic Inflammation, Elevated hs-CRP, and Oral Bacterial Pathogens Decrease After Two Years of Natural Dental Health Treatments: A Case Study - December 29, 2023
- Systemic Inflammation, Elevated hs-CRP, and Oral Bacterial Pathogens Decrease After Two Years of Natural Dental Health Treatments: A Case Study - November 8, 2019