I am going to ask the question, would you agree antibiotics can be bad but heart attacks are worse? As this is part 3 of my series, I hope I am hearing a unified “Yes”. In my opinion, systemic antibiotic should be used in an attempt to lessen the translocated pathogens. The high-risk patient is no longer capable of fighting, resisting, or diminishing the pathogenic loads on their own and the systemic antibiotic is an option. Yes there is a risk of antibiotic adverse reaction but a heart attack is worse. Here are some statistics to consider.
Antibiotics can be bad
- Annual antibiotic related deaths are reported from resistance reactions and/or allergic reactions.
- Resistance and allergic reactions are considered adverse reactions by some authorities.
- Some report antibiotic resistance as an adverse reaction only.
- In 2014 the CDC reports, the annual number of antibiotic doses prescribed to out-patients at 266.1M.[1]
- In 2016, they report the number had dropped to 154M.[2]
- The CDC reports that the annual death rate from antibiotic resistance is 23,000/year[3].
- Using 2014 total antibiotic doses prescribed, the death rate incidence would be about 8.6/100,000.
- Using a study from the New England Journal of Medicine a death rate for resistance for antibiotics in community, would be about 11/100,000.[4]
- Several reports state that antibiotics are responsible for about ½ all drug related allergy deaths.[5] [6]
- There are a few reports that assign annual allergy death numbers to drugs in general.
- Using Gomes study data from 2005, the annual incident rate for death from an antibiotic allergy reaction would be less than 50/100,000; using Jerschow’s work in 2014 the death incidence would be about 47/100,000.[7]
So, the total annual incidence of death from antibiotic use is about 58/100,000; including resistance and allergic. In conclusion, antibiotics can be bad.
Heart Attacks and Strokes are worse
- Annual incident rate for a heart attack is 560/100,000 for patients 45 years and older.[8]
- About 1/3 of heart attack victims die; this puts annual incidence of death from heart attack at about 187/100,000.
- Annual incident death rate for strokes is 41.7/100,000.[9]
So, the annual total heart attack and stroke incidence of death is about 228.7/100,000. In conclusion, heart attacks and strokes are worse.
Specific periodontal pathogens are now found causal to atherosclerotic disease and atherosclerotic disease is directly causal to heart attacks and strokes.[10] Research also shows that more than 5O% of cardiovascular events have a periodontal pathogen at its epicenter, directly associated with, or causal to that event.[11] [12] [13] Additional studies found a 50% increase in cardiovascular events occurs in the first four weeks following an invasive dental procedure, including SRP; this intimately connects pathogens to events.[14]
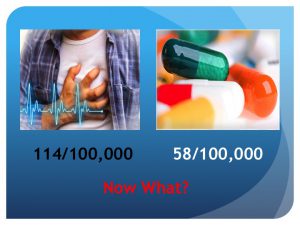
One half of heart attacks and strokes have been found to be directly connected to a specific oral pathogen; that fact would logically put the annual incidence of death related to this at about 114/100,000.
Doing the Math–Systemic antibiotics are bad but heart attacks are worse
The approximated annual death incident rate when systemic antibiotics are used is about 58/100,000.
The approximate annual death incident rate calculated for heart attack or stroke related to pathogens in a translocated micro-biome, is about 114/100,000.
The metrics we have available to review, show there is more risk from a cardiovascular event than from exposure to a systemic antibiotic. The election to use systemic antibiotics should be thoughtfully reviewed with all the data currently available, should be specific to a pathogen test result, and should be targeted at high-risk patients who are immune or genetically compromised. Much more research will evolve to facilitate the determination of best practices for the systemic mitigation of periodontal translocated mircro-biomes, until then, the use of systemic antibiotics has an important place.
[1]Measuring outpatient antibiotic prescribing, CDC 2014; cdc.gov/getsmart/community/pdfs/annual-report
[2] 1 in 3 antibiotic prescriptions unnecessary ; CDC, 2016, US Department of Health and Human Services. cdc.gov/getsmart/cdc newsroom
[3] Antibiotic resistance threats- Annual Report; 2013, CDC, US Department of Health and Human Services
[4] Lessa FC, Mu Y Bamberg WM, Beldavs ZG, Dumyati GK, Dunn JR, Farley MM, Holzbauer SM, Meek JI, Phipps EC, Wilson LE, Winston LG, Cohen JA, Limbago BM, Fridkin SK, Gerding DN, McDonald LC, et al. Burden of Clostridium difficile Infection in the United States. N Engl J Med 2015 Feb;372:825-834.
[5] Gomes,E, Demoly, P; Epidemiology of Hypersensitivity Drug Reactions; Curr Opin Allergy Clin Immunil. 2005; 5[4]:309-316
[6] Comprehensive study of allergic deaths in US finds medications are main culprit; Journal of Allergy and Clinical Immunology, Sept 2014
[7]Jerschow E, Comprehensive study of allergic death rates in US find medications are main culprit, Albert Einstien College of Medicine, report; Sept , 2014
[8] Mozaffarian D; Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation
[9] CDC; Summary health Statistics Tables for U.S. Adults: national Health Interview Survey, 2015. TableA-1
[10] Bale BF, Doneen AL, Vigerust DJ; High-risk periodontal pathogens contribute to the pathogenesis of atherosclerosis, Postgrad Med J,Nov, 2016,doi:10.1136/postgradmedj-2016-134279
[11] Gaetti-Jardim E, et. Al. Quantitative detection of periodontopathic bacteria in atherosclerotic plaques from coronary arteries. J Med Microbiol, 2009, 58[Pt 12], 1568-75.
[12] Figuero E, et. Al. Detection of periodontal bacteria in atheromatatous plaque by nested polymerase chain reaction. J periodontal. 2011, 82[10], 1469-77
[13] Pessi T, Bacterial signatures in thrombus aspirates of patients with myocardial infarction. Circulation,m2013, 127[11], 1219-28
[14] The rate of vascular events significantly increased in the first 4 weeks after invasive dental treatment and gradually returned to the baseline rate within 6 months. Annals of Internal Medicine 2010; 153:499-506;C Minassian, F D’Aiuto , A Hingorani, L Smeeth
For more information on how to become an OralDNA Provider – scan HERE: 
- “Words of Inspiration” by Dr. John Kempton - July 7, 2023
- Words of Wisdom from Dr. John Kempton - June 24, 2022
- Establishing New Treatment Objectives for Periodontal Disease - June 22, 2018
